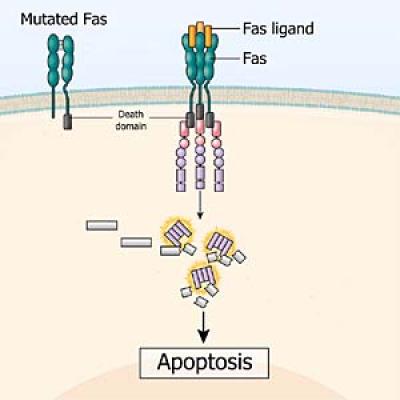
The Fas protein—which can be missing or defective in people with ALPS—spans the cell membrane and helps facilitate apoptosis, or programmed cell death. Without normal apoptosis, some cells can build up, thereby disrupting the immune system.
Autoimmune lymphoproliferative syndrome (ALPS) is a rare genetic disorder of the immune system first described by NIH scientists in the mid-1990s that affects both children and adults. In ALPS, unusually high numbers of white blood cells called lymphocytes accumulate in the lymph nodes, liver, and spleen and can lead to enlargement of these organs. ALPS can also cause anemia (low level of red blood cells), thrombocytopenia (low level of platelets), and neutropenia (low level of neutrophils, the most common type of white blood cell in humans). These problems can increase the risk of infection and hemorrhage.
Why Is the Study of Autoimmune Lymphoproliferative Syndrome (ALPS) a Priority for NIAID?
ALPS can cause debilitating symptoms and put those affected at an increased risk for developing serious health conditions, including autoimmune diseases and lymphoma. Researchers at NIAID are working to develop safe and effective treatments targeting the genetic defects in people with ALPS and related disorders.
How Is NIAID Addressing This Critical Topic?
Researchers at NIAID focus on gaining a better understanding of the clinical and genetic characteristics of people with ALPS and related disorders. By identifying the genes responsible for ALPS symptoms, NIAID researchers not only help affected families but also increase understanding of how the immune system works.
Related Topics
Primary Immune Deficiency Diseases (PIDDs)
There are more than 200 different forms of primary immune deficiency diseases (PIDDs) affecting approximately 500,000 people in the United States. These rare genetic diseases may be chronic, debilitating, and costly. Read about some of the individual PIDDs that NIAID is currently studying.
Autoimmune Diseases
More than 80 diseases occur as a result of the immune system attacking the body’s own organs, tissues, and cells. Some of the more common autoimmune diseases include type 1 diabetes, rheumatoid arthritis, systemic lupus erythematosus, and inflammatory bowel disease. Read about NIAID's research on autoimmune diseases.
Related Public Health and Government Information
To learn about resources for the diagnosis and management of ALPS and sources of support and advocacy, visit the National Library of Medicine, Genetics Home Reference autoimmune lymphoproliferative syndrome site.


