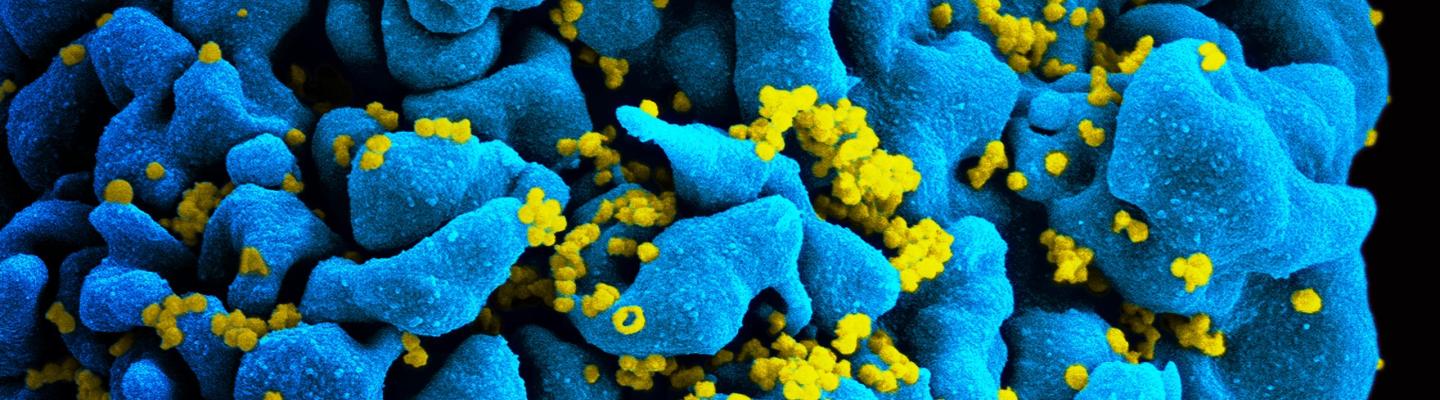
One of NIAID’s greatest success stories is that its research led to the development of numerous antiretroviral drugs to treat HIV/AIDS, turning what was once a uniformly fatal disease into a manageable chronic condition for many. NIAID is working to find new and more effective therapeutic products, drug classes, and combinations as well as safe and effective treatments for dangerous related co-infections and complications.
Antiretroviral Drug Discovery and Development
NIAID plays a role in many stages of the antiretroviral drug discovery and development process. The search for new drugs remains a priority due to the development of resistance against existing drugs and the unwanted side effects associated with some current drugs. NIAID supports basic research to identify novel strategies to prevent HIV from taking hold and replicating in the body, as well as preclinical research to formulate antiretroviral drugs that can be tested in people. In addition, NIAID supports the largest networks of HIV therapeutic clinical trial units in the world. Learn more about antiretroviral drug discovery and development.
Starting and Staying on Antiretroviral Treatment
Antiretroviral treatment has transformed HIV infection from an almost uniformly fatal infection into a manageable chronic condition. Starting daily antiretroviral therapy as soon as possible after diagnosis and staying on treatment are essential for keeping HIV under control, which benefits individual health and prevents HIV transmission to others. NIAID-supported research has played a key role in optimizing antiretroviral drug regimens and in establishing the importance of early treatment and strict adherence. Learn more about starting and staying on antiretroviral treatment.
Future Directions for HIV Treatment Research
A major goal of NIAID-supported research on HIV treatment today is to develop long-acting therapies that—unlike current antiretrovirals, which require daily dosing—could be taken only once a week, once a month, or even less often. Such long-acting therapies might be easier for some people to stick to than daily pills, and might also be less toxic and more cost effective. The three types of agents under study are long-acting drugs, broadly neutralizing antibodies, and therapeutic vaccines. Learn more about future directions for HIV treatment research.
HIV Treatment in Infants and Children
While rates of mother to child transmission of HIV have fallen over the last decade, the Joint United Nations Programme on HIV/AIDS (UNAIDS) still estimates that as many as 1.8 million children under 15 years old worldwide were living with HIV in 2017. NIAID supports research to determine which drugs, doses, and formulations comprise the safest and most effective HIV treatment regimens for pediatric patients, whose age, size, and organ function can cause them to react differently to medication than adults. Read more about HIV treatment in children. Learn more about HIV treatment in infants and children.
Treatment for HIV Co-Infections and Complications
In addition to medications that directly target the virus, people living with HIV may also receive therapy for complications and conditions associated with well-controlled HIV infection. These include medications to treat and prevent infections commonly seen in people living with HIV, such as viral hepatitis and tuberculosis, as well as noninfectious conditions, such as cardiovascular disease, certain cancers, and neurological disorders. Learn more about HIV co-infections and complications.
HIV Treatment, the Viral Reservoir, and HIV DNA
Antiretroviral therapy stops HIV from replicating (making copies of itself), but effective treatment does not completely eliminate the virus from the body. HIV lies dormant inside a small number of cells in the body, resulting in viral reservoirs. If treatment is stopped, these reservoirs can become active and start producing HIV. Learn more about HIV treatment, the viral reservoir, and HIV DNA.
Fact Sheet: 10 Things to Know About HIV Suppression
Achieving and maintaining a durably undetectable viral load by taking HIV medications daily as prescribed preserves the health of the person living with HIV and prevents sexual transmission of the virus to others. Learn more about HIV suppression.