NIAID supports university-based and pharmaceutical and biotechnology researchers who are working to develop new cholera treatments and vaccines to prevent infection. NIAID efforts to develop a preventive cholera vaccine have targeted two distinct but overlapping approaches: live and “killed” vaccines.
Protection Through Vaccination
Vaccination is an important way to protect vulnerable populations from cholera. Vaccines are usually evaluated in field studies by comparing the incidence of disease (in this case, cholera) in a vaccinated population to an unvaccinated placebo control population. An important re-analysis of a large study involving a vaccine containing inactivated cholera found that the incidence of cholera among the placebo recipients varied inversely with the level of vaccination in the community. The conclusion drawn was that vaccination reduced the amount of cholera in the environment, and therefore, the risk of infection to everyone in the community. This phenomenon, called community or “herd” immunity, occurs with many vaccines, and demonstrates the power of vaccination to quickly control and eliminate infectious disease, even when some in the population are not vaccinated. In the case of cholera, one epidemiological model in Bangladesh showed that because of community immunity, a vaccine containing inactivated cholera conferring relatively short-lived immunity could eliminate cholera entirely if 70 percent of the population was vaccinated.
Selected Papers
- Ali M, Emch M, von Seidlein L, Yunus M, Sack DA, Rao M, Holmgren J, Clemens JD. Herd immunity conferred by killed oral cholera vaccines in Bangladesh: a reanalysis. Lancet. 366(9479):44-9 (2005).
- Longini IM Jr, Nizam A, Ali M, Yunus M, Shenvi N, Clemens JD. Controlling endemic cholera with oral vaccines. PLoS Medicine.4(11):e336 (2007).
Live Vaccine Candidates in Development
The development of a vaccine containing live cholera involves reducing the bacteria’s virulence and ability to cause diarrhea while preserving its ability to induce an immune response. One candidate, Peru-15, developed by NIAID-funded researchers in the Harvard University laboratory of investigator John Mekalanos, Ph.D., has shown promise and is awaiting commercial sponsorship for final development and licensure. A second candidate, CVD-103HgR, was licensed in Europe, but is not currently in production or slated for use in cholera-endemic regions.
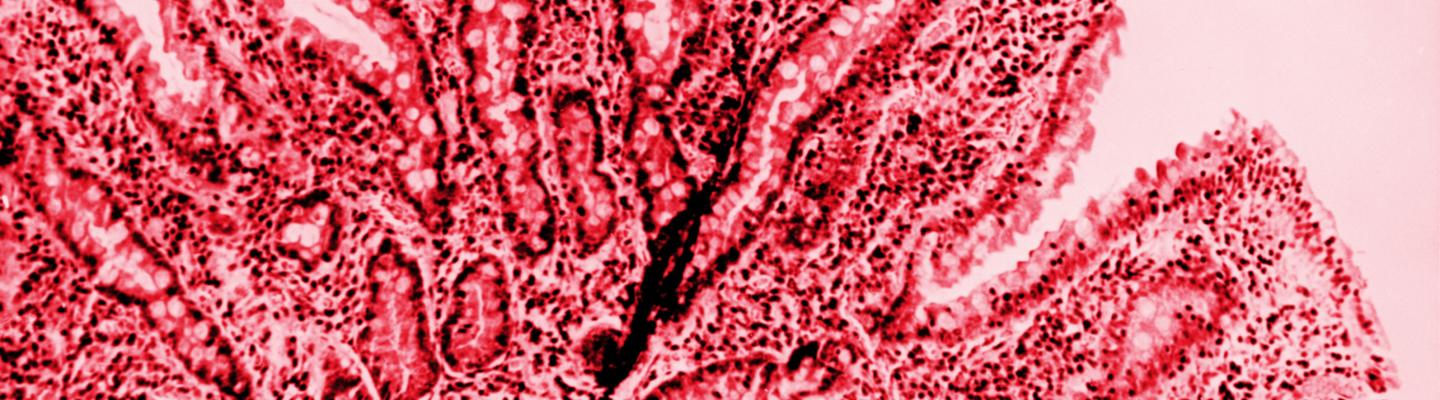
Killed Vaccines Being Used Internationally
“Killed” or inactivated vaccines are those that contain cholera bacteria that have been made harmless so as not to infect the vaccinated recipient. Currently, two of these types of cholera vaccines are available and both are administered orally as opposed to injection. Dukoral, developed by a Swedish research team led by Jan Holmgren, M.D., Ph.D., of the University of Gothenburg, is presently licensed in more than 60 countries and more than 10 million doses have been administered. The technology used to create Dukoral was later transferred to Vietnam and India, where a modified killed cholera vaccine is being produced as OCV-Vax in Vietnam and as Shanchol in India.
There are a number of advantages to these orally-administered killed vaccines, including their ease of administration, low cost, and current international licensure. If used on a broader scale, the vaccines could reduce global cholera rates, especially if antimicrobial and oral rehydration therapies are also available, and sanitation programs are supported by community education. There are challenges, however. For example, the current vaccines provide a short duration of protection; therefore, a control program with these vaccines may be difficult to sustain over the long term, particularly in resource-constrained countries.
Treatments
A man being treated for cholera.
Early Research Led to Today’s Most Important Treatment
Oral rehydration therapy (ORT), or the administration of an oral solution containing glucose and electrolytes, is currently the predominant treatment for cholera worldwide. According to the World Health Organization, up to 80 percent of cholera patients can successfully be treated by ORT alone; the remaining 20 percent require intravenous rehydration to ensure a full recovery.
New Research Explores Molecular and Folk Remedies

Sea buckthorn berries from Russia.
In addition to ORT, NIAID-funded researchers have found at the cellular and molecular levels other promising avenues for cholera treatment. Through an NIH Merit Award, a team led by Alan Verkman, M.D., Ph.D., of the University of California, San Francisco, studied the cystic fibrosis transmembrane regulator (CFTR), a chloride channel in the intestines that is activated during cholera infection. The team identified a family of small molecule inhibitors that prevent chloride secretion, which in turn inhibits diarrhea and reduces the loss of sodium and water that occurs during diarrheal episodes. Other intestinal ion channels may also be treated, including the calcium-activated chloride channel (CaCC), which has been implicated in other types of infection. One benefit of these inhibitors is that because they are active on the intestinal luminal surface and not necessarily absorbed into the body, they may have an inherently favorable toxicology profile.
One group of NIAID-funded researchers found that a folk remedy from the Amazonia region of Latin America, the Sangria do dragoderivative from the sap of the Croton lecheri tree from Peru, effectively inhibits both CFTR and CaCC. Similarly, NIAID grantees at Dartmouth Medical School are studying a major transcriptional regulator for cholera toxin expression and its possible relationship to the berry-bearing plant sea buckthorn. Further research into the molecular basis of microbial pathogenesis is leading to new discoveries explaining how these herbal and traditional medicines work.
Selected Papers
- Tradtrantip L, Namkung W, Verkman AS. Crofelemer, an antisecretory antidiarrheal proanthrocyanidin oligomer extracted from Croton lechleri, targets two distinct intestinal chloride channels. Mol Pharmacol. 77(1):69-78 (2010).
- Tradtrantip L, Namkung W, Verkman AS. Crofelemer, a novel agent for treatment of secretory diarrhea. Ann Pharmacother. 44(5):878-884 (2010).