There is a great need to develop rapid, point-of-care tests to determine whether people are infected with Borrelia burgdorferi, the bacterium that causes Lyme disease. NIAID is committed to improving Lyme disease diagnostics by supporting innovative research projects.
Priorities include finding potential targets—substances that new diagnostic tools might measure in patient samples—and improving the sensitivity and specificity of currently available diagnostic tests, thereby leading to more accurate results.
Important Considerations
Lyme disease can be difficult to diagnose for a number of reasons. Many of the common symptoms associated with the disease, such as headaches, dizziness, and joint/body pain, also occur with other diseases. The most distinct symptom of Lyme disease—the circular red rash known as erythema migrans (EM)—does not appear in at least one quarter of people who are actually infected with Lyme bacteria. Also, current diagnostic tests do not always detect early Lyme disease since antibodies take time to rise to detectable levels. Because treatment is generally more effective in early stages of the disease, it is important to develop new tools that can help doctors make an early diagnosis.
Doctors need to know whether a patient has an active infection, or has been exposed to the Lyme bacteria earlier in their life. Current diagnostic tests have some limitations that make a clear, quick diagnosis difficult.
Lyme antibody tests—the most common diagnostic tool available today—look for antibodies in the blood that show a person has been exposed to B. burgdorferi. But it can take a few weeks before a person's immune system creates measurable levels of antibodies. This gap between being infected with the bacteria and the body's creation of antibodies can result in a false negative test for those with very early Lyme disease, resulting in a delay in treatment.
Conversely, it is possible to receive a false positive test when a person does not actually have Lyme disease. Unfortunately, other bacterial infections may mistakenly be reported as a positive Lyme antibody test. These issues highlight the need for diagnostic tools that can distinguish between Lyme and other bacteria, and can find evidence of Lyme disease soon after infection.
Current Diagnostic Approaches
To diagnose Lyme disease, a healthcare provider usually uses laboratory tests approved by the Food and Drug Administration (FDA) combined with information about a patient’s symptoms.
The Centers for Disease Control and Prevention (CDC) currently recommends a two-tiered testing approach: a conventional enzyme-linked immunoassay (ELISA) test, followed by a Western Blot test. The ELISA is a blood test that detects antibodies but does not test for B. burgdorferi itself. A positive result from this first-level screening may suggest current or past infection. The ELISA is designed to be very “sensitive,” meaning that almost everyone who has Lyme disease (and some people who do not) will test positive. If the screening test is negative, it is highly unlikely that the person has Lyme disease and no further testing is recommended. If the screening test is positive or inconclusive, a Western blot test should be performed to confirm the results.
Used appropriately, the Western blot test is designed to be “specific,” meaning that it will usually be positive only if a person has been truly infected by B. burgdorferi. If the Western blot is negative, it suggests that the ELISA test was a false positive.
CDC does not recommend testing by Western blot without first using the ELISA. Using the Western blot on its own makes a false positive result more likely. Such results may lead to people being treated for Lyme disease when they do not have it, instead of being treated for the true cause of their illness.
Other Diagnostic Tests for Lyme Disease
Some laboratories offer Lyme disease testing using urine or other body fluids. These tests are not approved by FDA because they have not been proven to be accurate. For example, one study of urine-based polymerase chain reaction (PCR) assays for Lyme disease diagnosis showed that with currently available tools, urine cannot be used to accurately diagnose Lyme disease. Another study by NIAID-supported scientists showed that the Lyme Urinary Antigen Test (LUAT) was unreliable and resulted in excessive numbers of false positives. In the same study, researchers confirmed that an ELISA followed by a Western blot test was nearly 100 percent reliable in diagnosing Lyme disease. With the availability of so many Lyme disease tests, including non-commercial tests developed by individual facilities, it is impossible to address the accuracy of each one. The development of new, rapid, clearly validated diagnostic tests continues to be a need.
Current Research on New Approaches
NIAID actively supports research on Lyme disease diagnostics. Small businesses and public/private partnerships often submit applications for new research projects. NIAID grantees also work directly with CDC scientists to evaluate and compare the effectiveness of currently used diagnostic methods.
Working with CDC, NIAID plays a major role in encouraging the development of new approaches to improve Lyme disease diagnosis in people with tick-borne co-infections such as anaplasmosis or babesiosis. New diagnostic tests are also needed to distinguish between people with B. burgdorferi infection and those whose immune responses stemming solely from past Lyme disease vaccination. Although Lyme disease vaccines for humans are no longer available in the United States, the discontinued LYMErix vaccine used between 1998 and 2002 was based on a specific part of B. burgdorferi called outer surface protein A (OspA). In response to the vaccines, immunized individuals developed antibodies for OspA. Because the conventional ELISA measures OspA antibodies to determine if someone has Lyme disease, the test does not provide accurate results for immunized individuals. People who received the vaccination will test positive whether or not they are actually infected with B. burgdorferi.
NIAID is supporting research on a variety of approaches to improve the diagnosis of Lyme disease:
- The development and testing of a new cytokine-based immunoassay for Lyme diagnosis, if successful, could allow for earlier and more rapid diagnosis of Lyme disease.
- Several investigators are working on the development of a new, rapid point-of-care Lyme diagnostic test using lateral flow technologies.
- Metabolic biomarkers and biosignatures for improved diagnostics are being identified and characterized. These studies may contribute to new methods for detecting Lyme disease, earlier-stage diagnosis, accurate staging of disease, or indications of successful treatment. For earlier-stage diagnosis, rather than wait for the antibodies to appear in the blood, investigators looked at other molecules that arise earlier in infection. The researchers examined the pattern of a host of non-antibody molecules, or biomarkers, that increase in response to B. burgdorferi infection, and compared it to the pattern seen for other common diseases that share some overlapping symptoms with Lyme disease. They were able to identify a pattern of biomarkers that could differentiate early Lyme disease from the other illnesses tested, and could accurately diagnose the illness even in clinical samples that had tested negative by the current immunologic assay.
In 2017, the National Institutes of Health, CDC, and FDA hosted a webinar to provide updates on U.S. Department of Health and Human Services federal research on tickborne disease diagnostics.
Future Possibilities for Diagnostic Tools
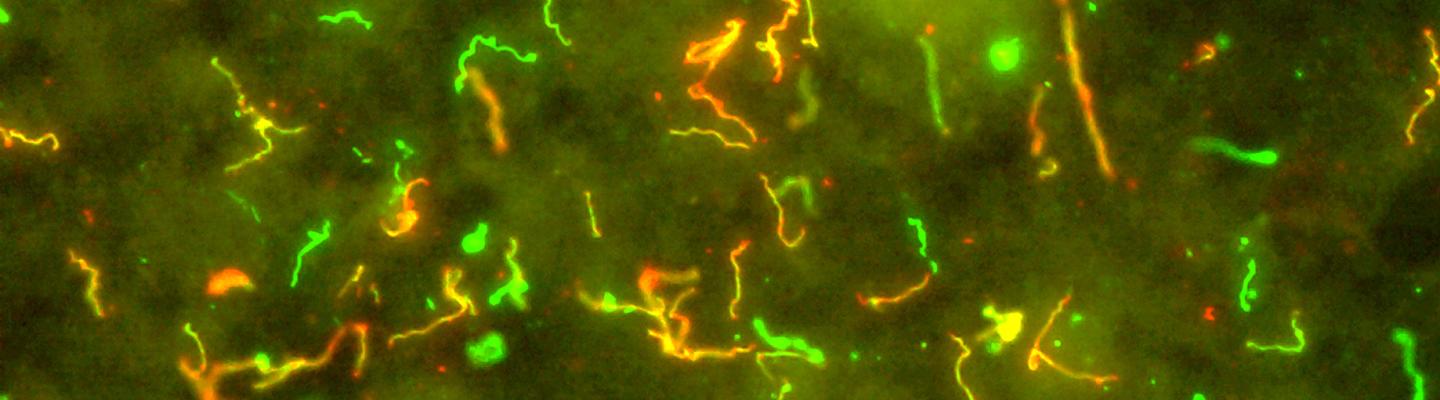
NIAID-supported scientists have identified genome sequences for multiple strains of B. burgdorferi. Greater advances in diagnostics are anticipated as genetic information is combined with advances in microarray technology, imaging, and proteomics. These growing fields of science are expected to lead to improved diagnostic tools as well as provide new insights on the pathogenesis of Lyme disease. Examples of tools being developed with NIAID support include use of metabolomics to characterize new biomarkers of infection, next generation T-cell based measurements, and novel antigens for improved measurement of effective treatment.
Scientific Advances
Differentiating Lyme disease from Southern Tick-Associated Rash Illness
May 28, 2021NIAID researchers are using metabolic biomarkers and biosignatures to distinguish Lyme disease from other diseases with similar symptoms, such as Southern Tick-Associated Rash Illness (STARI)