For early Lyme disease, a short course of oral antibiotics, such as doxycycline or amoxicillin, cures the majority of cases. In more complicated cases, Lyme disease can usually be successfully treated with three to four weeks of antibiotic therapy.
After being treated for Lyme disease, a minority of patients may still report non-specific symptoms, including persistent pain, joint and muscle aches, fatigue, impaired cognitive function, or unexplained numbness. These patients often show no evidence of active infection and may be diagnosed with post-treatment Lyme disease syndrome (PTLDS).
Multiple clinical trials, funded by NIH and others, have shown no benefit to additional IV antibiotic treatment in patients with Lyme disease, although the interpretation of those results have been challenged by some.
Clinical Studies
NIAID has funded three placebo-controlled clinical trials to learn more about the efficacy of prolonged antibiotic therapy for treating PLDS. The published results were subjected to rigorous statistical, editorial, and scientific peer review.
These trials were designed to ensure that several key parameters were addressed:
- The susceptibility of B. burgdorferi, the bacterium that causes Lyme disease, to specific antibiotics
- The ability of antibiotics to cross the blood-brain barrier, access the central nervous system, and persist at effective levels throughout the course of therapy
- The ability of antibiotics to kill bacteria living both outside and inside mammalian cells
- The safety and welfare of patients enrolled in the trials
The first clinical trial, which included two studies conducted at multiple research sites, provided no evidence that extended antibiotic treatment is beneficial. In those studies, physicians examined long-term antibiotic therapy in patients with a well-documented history of previous Lyme disease, but who reported persistent pain, fatigue, impaired cognitive function, or unexplained numbness. Patients were treated with 30 days of an intravenous antibiotic followed by 60 days of treatment with an oral antibiotic.
These studies reinforced the evidence that patients reporting PTLDS symptoms have a severe impairment in overall physical health and quality of life. However, prolonged antibiotic therapy showed no benefit when compared with groups who received placebo.
In another study, published in 2003, researchers examined the effect of 28 days of intravenous antibiotic compared with placebo in 55 patients reporting persistent, severe fatigue at least six months following treatment for laboratory-diagnosed Lyme disease. Patients were assessed for improvements in self-reported fatigue and cognitive function.
In that study, people receiving antibiotics reported a greater improvement in fatigue than those on placebo. However, no benefit to cognitive function was observed. In addition, six of the study participants had serious adverse events associated with intravenous antibiotic use, and four patients required hospitalization. Overall, the study authors concluded that additional antibiotic therapy for PTLDS was not supported by the evidence.
A subsequent study supported by the National Institute of Neurological Disorders and Stroke (NINDS), also part of the National Institutes of Health, showed that long-term antibiotic use for Lyme disease is not an effective strategy for cognitive improvement. Researchers studied 37 individuals with well-documented Lyme disease, at least three weeks of prior intravenous antibiotics, a current positive Lyme test (IgG Western blot), and self-reported memory impairment. Patients received either 10 weeks of intravenous ceftriaxone or intravenous placebo, and were examined for clinical improvement using objective memory tests. In a statistical model, the ceftriaxone group showed a slightly greater improvement at 12 weeks, but at 24 weeks both the ceftriaxone and the placebo groups had improved similarly from baseline. In addition, adverse effects attributed to intravenous ceftriaxone occurred in 26 percent of patients. The authors concluded that because of the limited duration of the cognitive improvement and the risks involved, 10 weeks of intravenous ceftriaxone was not an effective strategy for cognitive improvement in these patients, and more durable and safer treatment strategies are still needed.
A reappraisal of several of these studies concluded that IV antibiotics may provide benefit to PTLDS fatigue, but in light of significant adverse events they were not recommended and improved methods of treatment were needed. Another study challenged the interpretation of the results on statistical grounds, a position not accepted by the study authors. Individuals therefore continue to debate whether additional antibiotic treatment trials are needed, or if the lack of benefit from such an approach is settled science. Most recently, a clinical trial out of the Netherlands concluded that in patients with persistent symptoms attributed to Lyme disease, longer term treatment with antibiotics did not provide additional benefits compared with traditional treatment regimens. That study had two important differences from the previous trials. First, it addressed treatment for infection with the European Borrelia species B. garinii and B. afzelii. Second, it addressed previous criticisms of overly strict enrollment criteria for the other studies by broadening the diagnostic criteria required for enrollment. Despite these differences, the study results reinforced the conclusions of the earlier trials.
Currently, NIAID researchers are actively recruiting subjects for a clinical study that aims to use xenodiagnoses to detect Borrelia burgdorferi in patients who have been treated with antibiotics. NIAID scientists are also recruiting subjects for a clinical study that focuses on evaluating the clinical, microbiological and immunological characteristics of Lyme disease patients who may have been treated with antibiotics.
For more information, please see the Chronic Lyme Disease section.
Animal Models
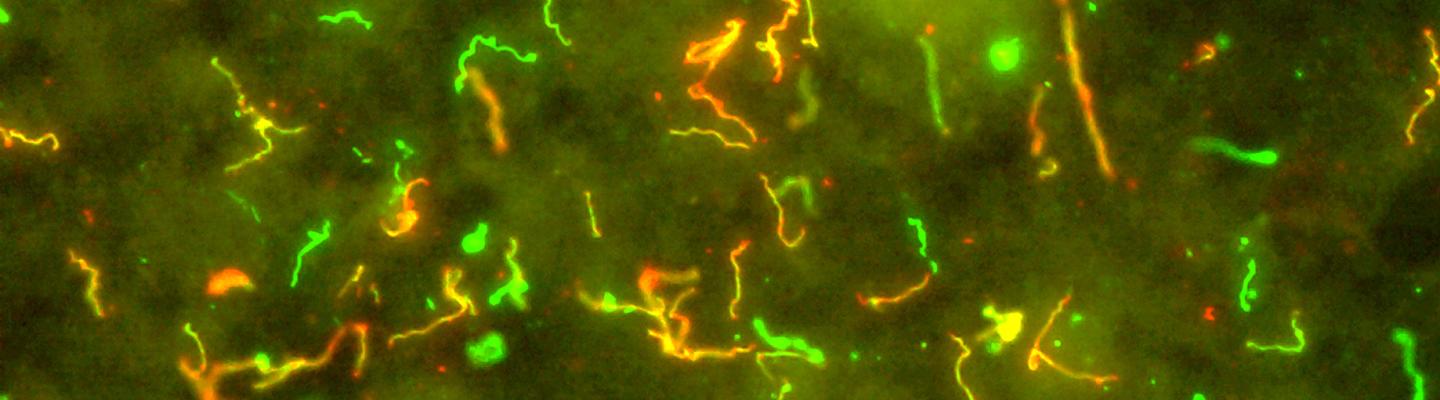
Animal models have provided considerable information on the transmission and pathogenesis of Lyme disease, as well as on the mechanisms involved in the development of protective immunity. Studies of the effects of antibiotic therapy in animals infected with B. burgdorferi have been conducted most often with mice but also with rats, hamsters, gerbils, dogs, and non-human primates.
NIAID-supported studies have shown that B. burgdorferi can be detected in mice for at least three months after treatment with therapeutic doses of various antibiotics (ceftriaxone, doxycycline, or azithromycin). In these studies, surviving bacteria could not be transmitted to healthy mice, and some lacked genes associated with infectivity. By six months, antibiotic-treated mice no longer tested positive for the presence of B. burgdorferi, even when their immune systems were suppressed. Nine months after antibiotic treatment, low levels of Borrelia DNA still could be detected in some—but not all—of the mice. These findings indicate that noninfectious B. burgdorferi can persist for a limited period of time after antibiotic therapy. The implications of these findings in terms of persistent infection and the nature of PTLDS in humans still need to be evaluated.
In a 2008 study, mice were treated with the antibiotic ceftriaxone for one month following either early or later stages of infection with B. burgdorferi. After completing antibiotic treatment, tissues from the mice were analyzed using a variety of scientific methods. B. burgdorferi could not be grown in cell cultures for any of the mice treated with antibiotics. In a small number of the treated mice, however, bacteria were detected in their tissues. Further, when Ixodes scapularis ticks fed on some of the antibiotic-treated mice, the ticks were able to transmit the bacteria to mice with weakened immune systems who were not previously infected with B. burgdorferi. Highly sensitive laboratory tests were able to detect the presence of B. burgdorferi in these mice. However, the bacteria did not grow in cell cultures. The implications of these findings in terms of persistent infection and the nature of PTLDS in humans are yet to be fully understood.
Several recent studies suggest that B. burgdorferi may persist in animals after antibiotic therapy. In one study, NIAID-supported scientists found that remnants of B. burgdorferi remained in mice after antibiotic treatment. Another team of NIAID-supported investigators found that intact B. burgdorferi persist in nonhuman primates after antibiotic treatment. It was not possible to culture these bacteria and it is not clear whether they are infectious. More recent work by replicated the earlier finding of persisting DNA but non-cultivatable B. burgdorferi after antibiotic treatment using a mouse model. Additional research is needed and continues to be supported by NIAID to learn more about persistent infection in animal models and its potential implication for human disease.
NIAID, in collaboration with NINDS, supported comprehensive studies on non-human primates looking at the neuropathology associated with post-treatment Lyme disease syndrome. A major goal of these studies was to optimize the Rhesus monkey model of Lyme disease as well as to determine the pathogenesis of the disease with a focus on its neurological manifestations.
The results of these studies have expanded the knowledge of those factors that contribute to the pathology associated with B. burgdorferi infection of the central nervous system. Among the findings are the following:
- Non-human primates are easily infected with low levels of B. burgdorferi through skin injection. In healthy non-human primates, the infection is transient and rapidly cleared as the animals developed antibodies to fight off infection. However, in non-human primates with suppressed immune systems, infection persists and involves the central and peripheral nervous systems, as well as organs, such as the heart, bladder, skin, and skeletal muscle.
- The presence of the bacteria’s genetic material was particularly prevalent in the central nervous systems of infected non-human primates compared to other tissues.
- The pattern of infection is dependent upon the strain of Borrelia used to induce infection; B. garinii induces a different type of disease in mice and non-human primates than does B. burgdorferi.