November 25, 2020
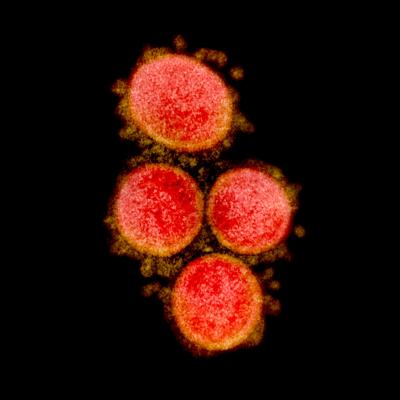
Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland.
The National Institute of Allergy and Infectious Diseases (NIAID), one of the National Institutes of Health, today announced that the fourth iteration of the Adaptive COVID-19 Treatment Trial (ACTT-4) has begun to enroll hospitalized adults with coronavirus disease 2019 (COVID-19) who require supplemental oxygen. The NIAID-sponsored trial will enroll up to 1,500 patients at approximately 100 sites in the United States and other countries.
Participants will be assigned at random to one of two treatment arms of equal size. One group will receive both dexamethasone, a corticosteroid available as a generic drug, and remdesivir, a broad-spectrum antiviral discovered and developed by Gilead Sciences, Inc., of Foster City, California. Remdesivir, also known as Veklury, was recently approved by the U.S. Food and Drug Administration (FDA) for the treatment of COVID-19 in hospitalized patients aged 12 years and older. The second group will receive remdesivir and baricitinib (brand name Olumiant), a modulator of inflammation that is approved by FDA to treat certain adult patients with moderate to severe rheumatoid arthritis. It was discovered by Incyte and licensed to Eli Lilly and Company (Indianapolis, Indiana). On November 19, FDA granted Emergency Use Authorization (EUA) for baricitinib in combination with remdesivir to treat suspected or laboratory confirmed COVID-19 in hospitalized patients aged 2 years and older who require supplemental oxygen, invasive mechanical ventilation, or extracorporeal membrane oxygenation.
The trial is blinded for the dexamethasone and baricitinib components, meaning investigators and participants will not know who is receiving dexamethasone and who is receiving baricitinib. Dexamethasone is administered by intravenous (IV) infusion, and baricitinib is a tablet taken orally. Therefore, one group will receive oral baricitinib tablets and an IV placebo, and the other group will receive IV dexamethasone and oral placebo tablets. All participants will receive intravenous remdesivir.
ACTT-1 began in February and tested remdesivir compared to placebo in hospitalized adult COVID-19 patients. Interim results, published in May, showed that remdesivir shortened the time to recovery. The ACTT-1 final results were published in the New England Journal of Medicine on November 5.
Baricitinib was tested in combination with remdesivir in ACTT-2, which enrolled 1,033 adults hospitalized with COVID-19. The primary results of this study were announced by Lilly in September, and peer-reviewed results are forthcoming. ACTT-2 findings indicated that the combination of baricitinib and remdesivir shortened the time to recovery relative to treatment with a placebo and remdesivir. The EUA of baricitinib was based, in part, on the FDA’s review of the data from the ACTT-2 trial.
Dexamethasone was evaluated in the global Randomized Evaluation of COVID-19 Therapy (RECOVERY) trial sponsored by the University of Oxford. Trial results showed that patients receiving dexamethasone demonstrated a lower mortality rate compared with patients receiving usual care.
To date, dexamethasone and baricitinib are the only two therapies that reduce inflammation that have demonstrated efficacy for the treatment of hospitalized adults with COVID-19 in large, randomized clinical trials. However, the differences in study populations, mortality rates and endpoint data collected in the ACTT-2 and RECOVERY trials make it difficult to make firm conclusions about the value of the interventions in various patient populations. ACTT-4 aims to determine whether baricitinib or dexamethasone, when administered with remdesivir, is more effective at preventing hospitalized adults on supplemental oxygen from progressing to requiring mechanical ventilation or death, among other outcomes, or if they are similar.
Investigators will assess participants’ clinical status daily using an 8-point ordinal scale ranging from a return to baseline pre-COVID-19 status and not hospitalized, to death. If discharged from the hospital, clinical status data will be collected during outpatient visits on days 15, 22, 29 and 60. The trial will evaluate the difference in the proportion of participants surviving without requiring invasive mechanical ventilation between the two treatment arms. A key secondary goal is to compare overall clinical status at day 15 in each group by comparing differences in the distribution of the 8-point ordinal scale in each group.
The trial is expected to take approximately three to four months to fully enroll. For more information about the trial, please visit clinicaltrials.gov and search identifier
NCT04640168.
Contact
To schedule interviews, contact:
NIAID Office of Communications
(301) 402-1663
NIAIDNews@niaid.nih.gov

