In 2019, scientists at NIAID and NIAID-funded institutions continued to make progress in understanding, preventing and treating allergic, immunologic and infectious diseases. This year saw advances in treating Ebola virus disease, developing gene therapy for a rare immunologic disorder, and understanding the causes of acute flaccid myelitis. Other work accelerated progress toward development of a universal flu vaccine, enhanced knowledge of organ transplantation among people with HIV, and provided new tools for studying human prion diseases. In addition, NIAID made strides toward ending the HIV epidemic in the United States and preventing tuberculosis, the leading infectious cause of death worldwide.
Ten selected science news highlights from 2019 are summarized below. All demonstrate how public investment in biomedical research drives scientific progress and benefits human health.
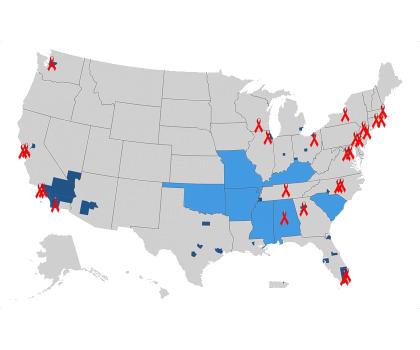
In September, NIH awarded approximately $11.3 million to 23 institutions across the United States to collaborate with community partners to develop locally relevant plans for diagnosing, treating and preventing HIV in areas with high rates of new HIV cases. These one-year pilot awards will help enhance the implementation science knowledge base needed for the proposed Ending the HIV Epidemic: A Plan for America. This bold new initiative aims to leverage the powerful data and tools now available to reduce new HIV diagnoses in the United States by 75% in five years and 90% by 2030.
Map showing the 48 counties, plus Washington, D.C., and San Juan, Puerto Rico, where >50% of HIV diagnoses occurred in 2016 and 2017, and an additional seven states with a substantial number of HIV diagnoses in rural areas. The red ribbons mark the locations of Centers for AIDS Research and AIDS Research Centers.
Credit: NIAID

NIAID and partners announced in August that individuals receiving the experimental Ebola treatments REGN-EB3 and mAb114 had a greater chance of survival compared to the experimental treatment ZMapp based on initial results from a clinical trial of Ebola therapeutics in the Democratic Republic of the Congo. Researchers published final results in the New England Journal of Medicine in November. The findings identify the first effective treatments for Ebola virus disease.
The Ebola treatment center (ETC) in Beni, Democratic Republic of the Congo. Operated by The Alliance for International Medical Action (ALIMA), the Beni ETC enrolled patients in the PALM study of Ebola therapeutics. The ETC is now operated by MSF.
Credit: ALIMA
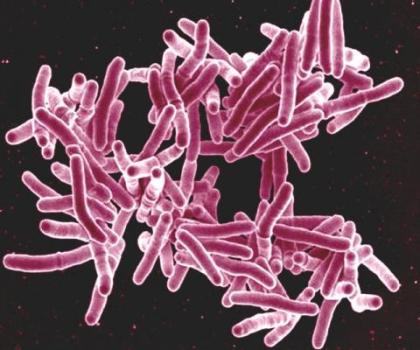
Tuberculosis (TB) remains the world’s leading infectious cause of death. Innovative new tools urgently are needed to stem the tide of TB and drug-resistant TB. This year, NIAID made investments in closing major gaps in TB prevention: protecting those in close contact with drug-resistant TB and developing improved TB vaccines. In June, NIAID announced the launch of a large TB prevention clinical trial for people exposed to multidrug-resistant TB. This fall, NIAID made contract awards to establish three new centers for TB immunology research to accelerate progress in TB vaccine development.
Scanning electron micrograph of Mycobacterium tuberculosis bacteria, which cause TB.
Credit: NIAID

This spring, NIAID began a clinical trial of an innovative universal influenza vaccine candidate known as H1ssF_3928. Developed by scientists at NIAID’s Vaccine Research Center, H1ssF_3928 is designed to teach the body to make protective immune responses against diverse influenza subtypes by focusing the immune system on a portion of the virus that varies relatively little from strain to strain. The Phase 1 trial is examining the vaccine’s safety and tolerability, as well as its ability to induce an immune response in healthy volunteers.
A healthy volunteer receives the H1ssF_3928 experimental universal influenza vaccine as part of a Phase 1 clinical trial at the NIH Clinical Center in Bethesda, Maryland.
Credit: NIAID
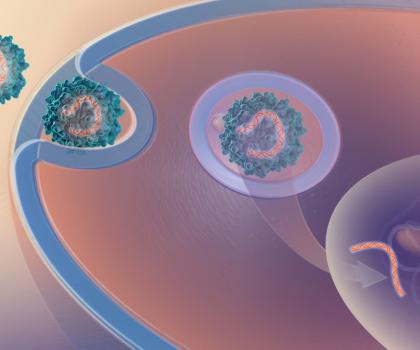
Researchers reported this spring that an experimental gene therapy co-developed by NIAID scientists can safely correct the immune systems of infants with X-linked severe combined immunodeficiency (X-SCID), a life-threatening inherited disorder in which infection-fighting immune cells do not develop or function normally. The design of the infant study was informed by encouraging early results from an ongoing NIAID clinical trial that is evaluating the gene therapy in older children and young adults with X-SCID who previously had received life-saving stem cell transplants but continued to experience complex medical problems.
Gene therapy involves inserting a healthy gene into the patient’s cells using a harmless virus as a carrier, or “vector.” Scientists developed a novel vector known as a lentivector for the X-SCID gene therapy.
Credit: NHGRI

Researchers reported in March that new HIV cases had declined by 30% in southern African communities where health workers conducted house-to-house voluntary HIV testing, referred people who tested positive to begin HIV treatment according to local guidelines, and offered other proven HIV prevention measures to those who tested negative. The results of this NIH-funded study, as well as other studies involving related strategies, suggest that universal “test and treat” approaches could help control the HIV epidemic in certain settings.
A study health worker draws blood from the finger of a study participant for an in-home HIV test.
Credit: Kim Cloete
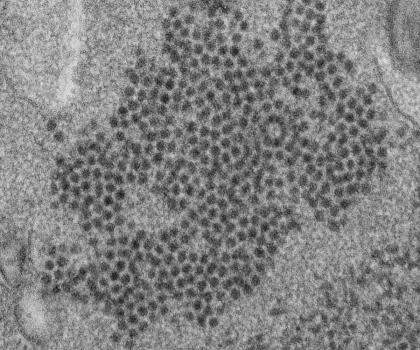
A NIAID-funded study provided additional evidence for an association between acute flaccid myelitis (AFM), a rare but often serious condition that causes muscle weakness and paralysis, and infection with non-polio enteroviruses. Spikes in AFM cases, primarily in children, have coincided in time and location with outbreaks of the enteroviruses EV-D68 and EV-A71, both of which typically cause mild respiratory illness. Scientists detected enterovirus-specific antibodies in samples of cerebrospinal fluid from 11 of 14 people with AFM, providing further evidence that enterovirus infection may be a factor in AFM.
An electron micrograph of a thin section of EV-D68, showing the numerous, spherical viral particles.
Credit: CDC
People living with HIV in South Africa who received kidney transplants from deceased donors with HIV had high rates of overall survival and kidney graft survival after five years, an international research team reported in October. In the United States, such transplants recently were legalized by passage of the HIV Organ Policy Equity (HOPE) Act of 2013, which permits U.S. transplant teams with an approved research protocol to transplant organs from donors with HIV into qualified recipients with HIV. In February, NIAID launched a liver transplantation study, which complements a kidney study launched in 2018, to compare clinical outcomes among people living with HIV in the United States who receive organs from deceased donors with HIV to those who receive HIV-negative organs.
AIDS awareness ribbons
Credit: NIAID
This fall, NIAID initiated the Collaborative Influenza Vaccine Innovation Centers (CIVICs) program, a new network of research centers that will work together to develop broadly protective and longer-lasting influenza vaccines. The CIVICs network will develop so-called universal influenza vaccines and explore approaches to improve seasonal influenza vaccines. These advances could substantially reduce influenza hospitalizations and deaths in the future.
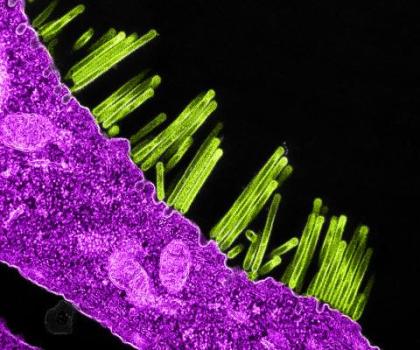
A colorized transmission electron micrograph of swine flu virus particles (green) budding from the surface of a cell (pink).
Credit: NIAID
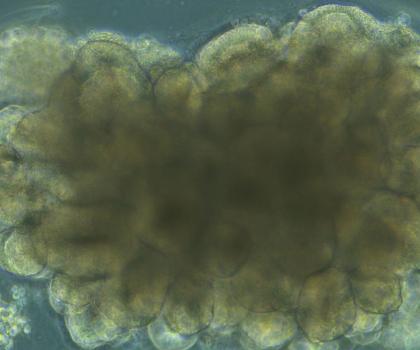
Scientists at NIAID’s Rocky Mountain Laboratories used human skin cells to create a "cerebral organoid" system to study Creutzfeldt-Jakob disease (CJD), a fatal neurodegenerative brain disease believed to be caused by prions. Cerebral organoids are small balls of human brain cells with similar organization, structure and electrical signaling to brain tissue. The researchers discovered how to infect cerebral organoids with prions using samples from two patients who died of CJD. Aided by this new model system, the researchers ultimately hope to learn how to prevent cell damage and restore the function of cells damaged by prion infection.
Brightfield microscope image of an organoid during development, showing highly structured regions forming.
Credit: NIAID

