How Children are Helping Scientists Battle a ‘List of Bad Viruses’
EV-D68 Pilot Project Could Guide Future Pandemic Preparedness
A group of children who recently began participating in a pilot study of a single rare viral disease could eventually provide NIAID scientists and colleagues with the recipe to help slow or stop future viral pandemics.
Researchers at four United States locations are enrolling children 10 and younger in a minimum 3-year study of enterovirus D68 (EV-D68), which evidence suggests can cause a polio-like neurologic disease in children called acute flaccid myelitis, or AFM. The disease was first identified in 2014 with most cases occurring every-other year in children during late summer and early fall. In 2018, physicians reported 238 AFM cases in the United States. Most cases involve fever and breathing difficulty that progress to sudden onset of limb weakness, loss of muscle tone, and loss of reflexes.
More broadly, the study is a test case for how some scientists think nations could plan for viral pandemics, using a two-step approach of meshing human immunology with virus sequence surveillance.
The national EV-D68 pilot study is part of PREMISE, the Pandemic Response Repository through Microbial and Immune Surveillance and Epidemiology. PREMISE is an initiative from NIAID’S Vaccine Research Center (VRC) that began in early 2021.
“We have to start somewhere,” Dr. Daniel Douek said about the EV-D68 pilot study, then explained the ultimate objective of PREMISE: “It sounds a little cheeky, but the aspirational goal is to measure immunity in every single human being on Earth against every single potential pathogen on Earth.” Douek is a VRC physician and researcher who oversees a program studying human immunology.
He is also co-director of PREMISE with VRC colleague Dr. Adrian McDermott. The PREMISE initiative comprises a network of investigators that aim to collect samples from groups of people to detect immunity against viruses of pandemic potential. PREMISE will also sequence samples from animals known to carry diseases that can transmit to people and people with symptoms to detect viruses.
Douek said the PREMISE initiative grew out of weekly discussions he and McDermott had with epidemiologist colleagues at Princeton University, Bryan Grenfell and C. Jessica Metcalf, a year before the COVID-19 pandemic began.
“They are disease ecologists, interested in population susceptibility, who wanted to know more from us about immunology,” Douek said. When COVID-19 hit, the group realized “we don’t need to just measure immunology, we need to translate that knowledge into products.”
They and collaborators are hoping PREMISE will show that, as Douek explained, it is possible to select a virus, learn how it infects, replicates and mutates; learn what makes certain people susceptible to infection; learn what protects other people from infection; and then use that data to inform the development and testing of vaccines and antibody products to have “waiting on the shelf” if needed. He said retired VRC scientist Dr. Barney Graham suggested EV-D68 as the perfect virus for a pilot study: the virus is a priority pathogen, it affects children, and scientists need to understand its transmission patterns post-COVID-19.
As of May 18, the EV-D68 study had enrolled 117 children. Participating sites include the University of North Carolina in Chapel Hill, University of Colorado/Colorado Children’s Hospital in Aurora, Weill Cornell Medical College in New York, and the University of Alabama-Birmingham.
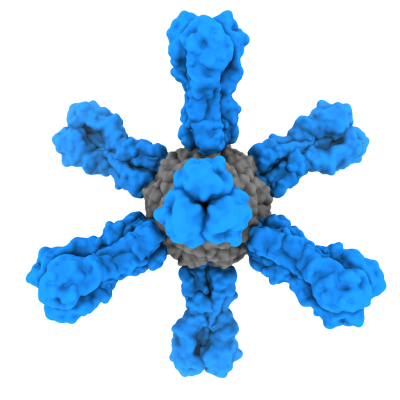
The pilot study will monitor participants for EV-D68 and other infectious diseases of interest using blood samples, and possibly a nasal swab, that are screened in the lab for beneficial immune-system proteins. Study findings will aid in understanding the seroepidemiology – for example which antibodies are most helpful – of EV-D68 and other infectious diseases. The resulting analyses will be shared to pre-emptively generate research and data resources for early detection and diagnosis, and to inform the identification of monoclonal antibody therapies and immunogens for vaccine discovery and development. These data will help guide the future of PREMISE.
If the EV-D68 pilot project is effective, Douek says researchers would apply the concept to a “list of bad viruses,” which includes hantaviruses, coronaviruses, influenza and various hemorrhagic fever viruses among others – all priority pathogens considered to have pandemic potential.
He is confident in the PREMISE concept because a related project with another Princeton team already is producing intriguing results from the Turkana region of Kenya. Douek says scientists are screening local participant samples against all known coronaviruses.
“We’re seeing some interesting things,” he said, adding that once the data are analyzed and interpreted, scientists plan to publish results that could help better understand how pathogens circulate among isolated populations. “Then it’s a question of pre-positioning with products that can benefit people.”
References:
H Nguyen-Tran, et al. Enterovirus D68: A Test Case for the Use of Immunologic Surveillance to Develop Tools to Mitigate the Pandemic Potential of Emerging Pathogens. The Lancet Microbe. (2022).
MJ Mina, et al. A Global lmmunological Observatory to meet a time of pandemics. Elife. (2020).