The first Food and Drug Administration approval of a treatment for eosinophilic esophagitis, announced in May 2022, marked a vital achievement not only for people with the disease, but also for scientists including a NIAID grantee whose research helped lay a foundation for this milestone.
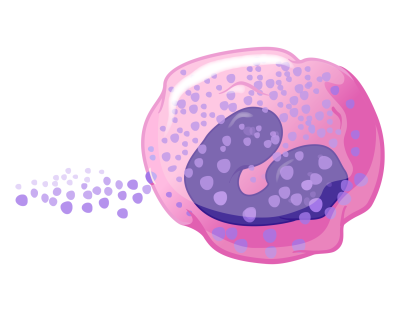
Eosinophilic esophagitis, or EoE, is a chronic disease characterized by an overabundance of a specific type of white blood cell, an eosinophil, in the esophagus. The disease is driven by allergic inflammation due to food. This inflammation damages the esophagus and prevents it from working properly. For people with EoE, swallowing even small amounts of food can be a painful and worrisome choking experience. EoE is the most common reason people must go to emergency departments for a healthcare provider to remove food stuck in their esophagus. People with EoE are often left to contend with the frustration and anxiety of a sometimes-lengthy list of foods to avoid, a poor quality of life, and a higher risk of depression. In severe cases, a feeding tube may be the only option to ensure proper caloric intake and adequate nutrition. About 160,000 people in the United States are living with EoE.
NIAID funding enabled Marc E. Rothenberg, M.D., Ph.D., at Cincinnati Children’s in Ohio to conduct basic and preclinical research starting in 1999 that uncovered the molecular cause of EoE. This finding suggested the type of drug needed to treat the disorder.
Before 2001, some in the medical community thought EoE was a form of acid reflux disease. Dr. Rothenberg’s lab published a paper that year establishing that EoE is actually an allergic disorder. The paper showed that mice exposed to an inhaled respiratory allergen developed EoE. This helped focus subsequent studies of EoE on the role of allergic inflammation.
A few years later, two seminal papers from Dr. Rothenberg’s lab identified the molecular changes taking place in the esophagus of people with EoE and showed that a cell-signaling molecule called IL-13 was responsible for many of those changes. IL-13 and another cell-signaling molecule, IL-4, together drive allergic inflammation in many diseases.
The first of these two key papers reported the results of an analysis of gene expression in cells on the lining of the esophagus in people with and without EoE. The study identified 574 genes that were copied into RNA “transcripts”—the instructions for making proteins—in greater or smaller numbers in people with EoE than in healthy people. This EoE transcript signature, or transcriptome, served as a key reference for subsequent studies of the disorder.
The second paper demonstrated in 2007 that many of the EoE-associated genes identified in the earlier paper are directly activated by IL-13 in cells lining the esophagus, implicating this molecule as a major regulator of the biological pathways involved in EoE. This finding suggested that IL-13-blocking drugs might effectively treat the disease. The study further showed that 98% of the EoE transcriptome reverted to normal levels of gene expression in people whose EoE was successfully treated with a class of steroid hormones called glucocorticoids. This indicated that the EoE transcriptome changes in response to changes in signs and symptoms of the disease. Dr. Rothenberg and colleagues therefore proposed using the EoE transcriptome to monitor the efficacy and mechanism of action of IL-13-blocking drugs at the molecular level.
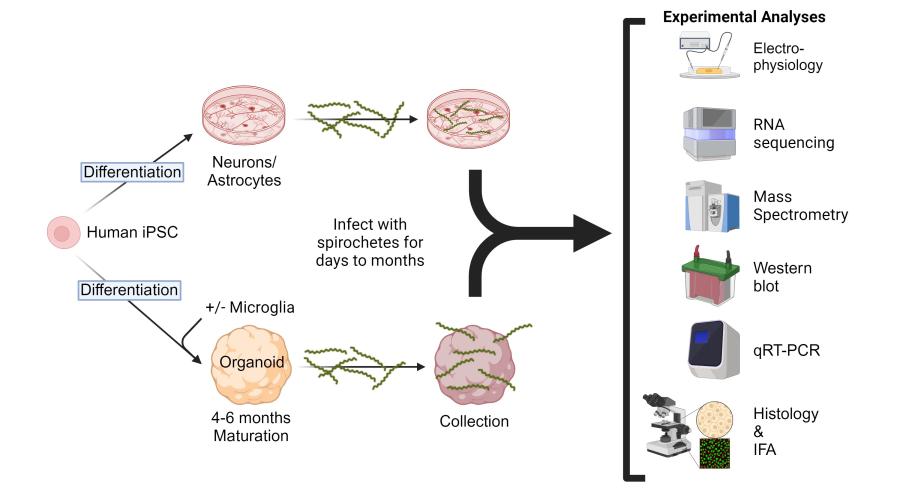
Several years later, Dr. Rothenberg designed and led the first clinical trial to test the efficacy of an anti-IL-13 monoclonal antibody for treating EoE. The investigators found that the antibody lowered levels of eosinophils in the esophagus and returned the expression of 29 key genes in the EoE transcriptome to normal levels in most treated participants. This and related molecular analyses from the trial, funded by Novartis Pharma AG of Basel, Switzerland, further supported Dr. Rothenberg’s theory that EoE was driven by IL-13.
These findings contributed to a body of foundational EoE research developed by a multitude of scientists and physicians. This scientific foundation, among many other factors, led Regeneron Pharmaceuticals Inc. of Tarrytown, New York, and Sanofi of Paris to begin testing one of their drugs for the treatment of EoE. The drug, a monoclonal antibody called dupilumab, works by blocking both IL-13 and IL-4.
Ultimately, Regeneron and Sanofi conducted a Phase 3 clinical trial showing dupilumab substantially improved the signs and symptoms of EoE compared to a placebo. Based on these results, FDA approved dupilumab for the treatment of the disease on May 20, 2022, making it the first medicine specifically indicated to treat EoE in the United States.
NIAID-funded basic and translational research continues to contribute to the development of preventive and therapeutic strategies for dozens of allergic, immunologic, and infectious diseases.
References:
A Mishra, et al. An etiological role for aeroallergens and eosinophils in experimental esophagitis. The Journal of Clinical Investigation DOI: 10.1172/JCI10224 (2001).
C Blanchard, et al. Eotaxin-3 and a uniquely conserved gene-expression profile in eosinophilic esophagitis. The Journal of Clinical Investigation DOI: 10.1172/JCI26679 (2006).
C Blanchard, et al. IL-13 involvement in eosinophilic esophagitis: Transcriptome analysis and reversibility with glucocorticoids. Journal of Allergy and Clinical Immunology DOI: 10.1016/j.jaci.2007.10.024 (2007).
ME Rothenberg, et al. Intravenous anti–IL-13 mAb QAX576 for the treatment of eosinophilic esophagitis. Journal of Allergy and Clinical Immunology DOI: 10.1016/j.jaci.2014.07.049 (2015).