A NIAID-supported study has found that respiratory syncytial virus (RSV) infection in the first year of life is associated with a significantly increased risk of asthma in children. The study was published in the journal The Lancet. These findings provide additional evidence for a casual association between the occurrence of RSV infection in children younger than 1 and an increased incidence of wheezing and asthma in later in life.
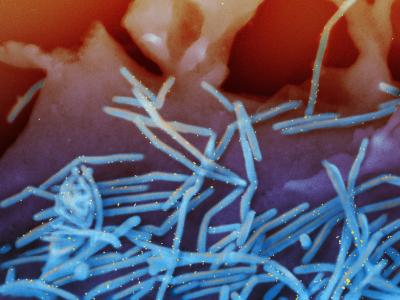
RSV is a seasonal respiratory pathogen that affects almost all children by age 2, and repeatedly throughout life. In most children, symptoms of the virus are mild and usually resolve within a week. However, RSV can lead to death or serious illness, especially in premature or very young infants, and those with chronic lung disease or congenital heart disease, although about half of all RSV hospitalizations are among healthy infants. In infants (children younger than 1), RSV is the leading cause of bronchiolitis, a lower respiratory tract infection in infants and young children presenting with coughing and wheezing. Prior evidence on the links between RSV infection in infancy and respiratory health derives from studies of children with severe RSV bronchiolitis, which impacts a minority of children. The population-level asthma risk following RSV infection of any severity has not been studied before.
The “Infant Susceptibility to Pulmonary Infections and Asthma Following RSV Exposure (INSPIRE)” is the first cohort specifically designed to test the hypothesis that not being infected with RSV in infancy decreases the risk of childhood asthma. The population-based cohort study included 1,946 healthy infants born between June and December of 2012 and 2013 who were 6 months old or younger at the beginning of the RSV season (November to March in the study area of Tennessee). Biweekly surveillance and serology tests were used to classify infants as RSV infected or not infected in the first year of life. Of the 1,741 who received classifications, 54% were infected with RSV in the first year of life.
Participants were followed prospectively for five years and then evaluated for 5-year current asthma, which was defined as 1) a parental report of diagnosed asthma or the use of asthma medications before age 5, and 2) any of the following in the 12 months prior to the 5-year visit: asthma symptoms, use of systemic (oral or intravenous) steroids for asthma, or doctor or emergency room visits for asthma symptoms.
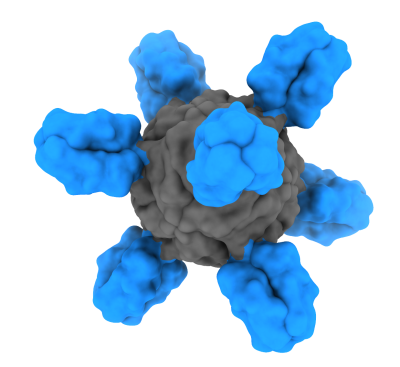
The study found that infants who were not infected with RSV in the first year of life had a 26% lower risk of asthma at 5 years of age than those who were infected with RSV as infants. Because the study was observational, the results do not definitively establish causality but do support a need for long-term follow-up of common respiratory outcomes among children in clinical trials of RSV prevention products.
Infancy is a critical time for immune system and pulmonary development; understanding how RSV infection before age 1 is associated with an increased risk of childhood asthma could help to prevent long-term childhood respiratory morbidity.
The study was funded by NIAID, the National Heart, Lung and Blood Institute, the National Center for Advancing Translational Sciences and the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Reference: C Rosas-Salazar, et al. Respiratory syncytial virus infection during infancy and asthma during childhood in the USA (INSPIRE): a population-based, prospective birth cohort study.
The Lancet DOI: 10.1016/S0140-6736(23)00811-5 (2023)