Apply to NIAID’s notice of funding opportunity (NOFO) Research Initiative for Vaccine and Antibiotic Allergy (UG3/UH3, Clinical Trial Not Allowed) for funding to conduct research that enhances understanding of antibiotic and vaccine allergies.
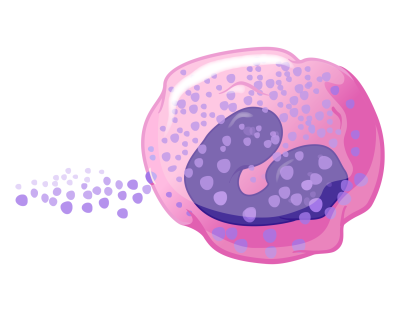
Allergic reactions to drugs and vaccines are a serious public health concern that causes wide and varied reactions, which include not only Immunoglobulin E (IgE)-mediated reactions, but other immune-mediated, largely unpredictable drug and vaccine reactions. An antibiotic allergy can lead to use of alternative, more expensive antibiotics, which may reduce efficacy and increase mortality in patients. Additionally, vaccine allergies can contribute to vaccine hesitancy, creating a public health issue.
Objectives
This NOFO seeks innovative projects to study the mechanisms and management of vaccine or antibiotic drug allergy (research on allergic responses to anti-viral, anti-fungal, and anti-parasitic drugs are also valid for consideration).
The scope of research into antibiotic or vaccine allergic reactions includes the following:
- IgE-mediated and other mechanisms of immediate allergic antibiotic or vaccine reactions.
- Non-IgE-mediated urticarial reactions to antibiotics or vaccines.
- Delayed-type hypersensitivity reactions to antibiotics or vaccines.
- Severe cutaneous adverse antibiotic or vaccine reactions.
- Biomarkers to identify people at risk for reaction or to confirm reactions to specific antibiotics or vaccines.
- Host factors that may predispose to allergic reactions including, but not limited to, host microbiome, genetics, or inflammatory conditions.
- Mechanisms by which specific infections may increase the risk of an allergic reaction to an antibiotic or vaccine.
- Immunomodulatory approaches to treating or preventing immunologic adverse antibiotic or vaccine reactions.
A secondary objective of this NOFO is to expand the number of investigators working in the field of vaccine and antibiotic drug allergy. We strongly encourage early-stage investigators to apply.
UG3/UH3 Phase Transition and Milestones
This funding opportunity is designed as a two-stage cooperative agreement in which NIAID project scientists will work with the investigative teams. Projects must be organized into a 2-year UG3 phase followed by a 3-year UH3 phase. The UG3 phase may include pilot, observational, or hypothesis-generating high-risk projects.
Preliminary data may be helpful but are not required within the application. You may propose to use electronic health records to identify potential participants for mechanistic studies. You are encouraged to use human samples such as those related to the clinically indicated and routinely used interventions or tests.
The UG3 phase must include milestones to determine the success of the project at the end of this phase. Milestones may be negotiated or re-negotiated after award as this program includes the flexibility to quickly revise milestones or aims within the scope of the original peer-reviewed application. Following the completion of the UG3 phase, NIAID staff will review the progress made and determine whether the project will continue to the UH3 phase.
NIAID support for the UH3 phase is contingent upon progress made during the UG3 phase, meeting the milestones, programmatic priorities, the original UG3/UH3 peer review recommendations, and the availability of funds. Some projects might not transition from the UG3 to the UH3 phase. Projects supported by the UH3 phase are hypothesis driven, mechanistic, and should extend the work initiated by the UG3 phase.
Nonresponsive Research Topics
NIAID will consider applications that propose the following topics to be nonresponsive and not review them:
- Adverse drug reactions that are predictable or related to pharmacologic properties of the drug such as toxicity or overdose.
- Investigation into drugs that are not antibiotics or vaccines (however, research on anti-viral, anti-fungal, and anti-parasitic drugs is allowed).
- Investigations into Guillain-Barré Syndrome or drug-induced autoimmune reactions.
- Investigations of central nervous system and other neurologic adverse responses.
- Investigations into the pathogens rather than host allergic responses to the antibiotics or vaccines.
- Applications that do not propose mechanistic research in the UH3 phase.
- Vaccines that are administered via a route that is not FDA approved.
- Vaccines that are used as an immunotherapeutic (e.g., allergen immunotherapy).
- HIV/AIDS research.
Additionally, applications that do not describe a 2-year UG3 phase and a 3-year UH3 phase in the research strategy will be considered nonresponsive and will not be reviewed.
Award and Budget Information
NIAID will fund four or five awards in fiscal year 2025. Application budgets are not expected to exceed $250,000 in annual direct costs and must reflect the actual needs of the proposed project.
The proposed project period for the initial phase (UG3) must be 2 years and the proposed project period for the subsequent phase (UH3) must be 3 years, with the total project period being 5 years.
Deadline
Submit your application by June 21, 2024, at 5 p.m. local time of the applicant organization.
Send any inquiries to Dr. Patricia Fulkerson, NIAID’s scientific contact, at patricia.fulkerson@nih.gov or 202-641-4535. Send questions about peer review to Dr. Poonam Tewary at poonam.tewary@nih.gov or 301-761-7219.