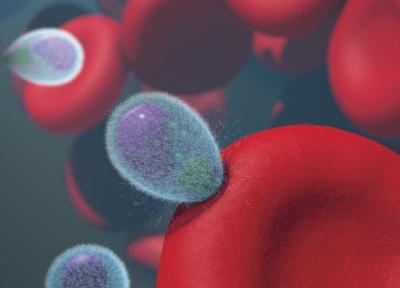
For years, malaria vaccine developers have focused on thwarting a key moment in the malaria parasite’s life cycle: when two parasite proteins, AMA1 and RON2L, combine to form a complex that anchors the parasite to a red blood cell and eases its passage into the cell interior. Quite sensibly, researchers developed candidate vaccines that elicit antibodies capable of blocking the crucial attachment. However, because AMA1’s make-up varies widely among different parasite strains, any vaccine based on a single strain’s AMA1 cannot protect against other parasite strains and thus has limited usefulness in malaria-endemic countries. Experimental malaria vaccines have also been made by mixing AMA1 and RON2L proteins. While these do elicit more strain-transcending antibodies than AMA1-only vaccines, they are difficult to manufacture and simple mixtures of AMA1 and RON2L in vaccines do not form the kind of stable protein complex seen in nature.
Now, researchers in NIAID’s Laboratory of Malaria Immunology and Vaccinology have used structural information about the two parasite proteins along with mechanistic information about the interaction between AMA1 and RON2L to design and build an entirely novel immunogen (the component of a vaccine that elicits an immune response). When tested in rats, their “structure-based design 1” (SBD1) immunogen vaccine performed better than any AMA1 or AMA1-RON2L vaccine. It also upends the conventional wisdom that successful vaccines must elicit receptor-blocking antibodies, notes Niraj H. Tolia, Ph.D., who led the research team.
The SBD1 immunogen does not exist in nature, explains Dr. Tolia. Rather, it consists of AMA-1 that the team altered by rearranging its amino acid sequence in a way that they predicted would work well as a vaccine. Once altered, the scientists linked RON2L to a position in their immunogen to recreate the two protein AMA1-RON2L complex. The team analyzed the structure of the designed immunogen using X-ray crystallography and determined that it closely mimicked that of naturally occurring AMA1-RON2L complex. However, SBD1 has a number of advantages over a simple mixture of two component proteins, Dr. Tolia explains. For instance, it is highly stable once injected, is easy to manufacture in large quantities and consistently takes the desired, immune-stimulating shape.
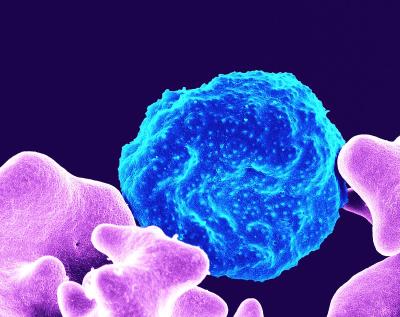
In rats, SBD1 vaccine elicited significantly more potent strain-transcending antibodies than either AMA1 alone or an AMA1-RON2L complex vaccine. The ability to provide protection from multiple parasite strains is highly desirable for any malaria vaccine. Most surprisingly, Dr. Tolia says, the SBD1 vaccine provided this strain-transcending protection even though it generated no antibodies whatsoever that were aimed at blocking AMA1 from binding to RON2L and initiating attachment to the red blood cell. Instead, it appears SBD1 elicits high quality antibodies that inhibit parasite growth by targeting parts of the parasite’s proteins that lie outside of RON2L binding site and operate independently of receptor blockade, explains Dr. Tolia.
Together, the team’s observations about SBD1 make it an appealing candidate for further studies in animals and perhaps ultimately in human trials, he adds. Furthermore, other parasites, including those that cause the human diseases toxoplasmosis and babesiosis and one that causes disease in cattle and dogs, use their own forms of AMA1 protein to invade host cells. Thus, insights gained in this recent work may be applicable to the design of vaccines against those parasites as well.
Reference: PN Patel et al. Structure-based design of a strain transcending AMA1-RON2L malaria vaccine. Nature Communications. DOI: 10.1038/s41467-023-40878-7 (2023).