Country-led genetic analysis of samples collected through the Republic of Congo (RoC) epidemiologic surveillance system in early 2024 showed that mpox was affecting people in parts of the country where it has not been historically reported, and point to increases in human-to-human transmission across the border with the neighboring Democratic Republic of the Congo (DRC), where a large outbreak was declared a public health emergency of international concern in August of the same year. The analysis was conducted by the RoC Laboratoire National de Santé Publique (LNSP) in Brazzaville with support and scientific partnership from NIAID and was published in The Lancet.
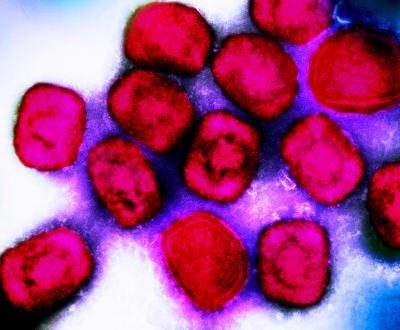
There are two known types or “clades” of monkeypox virus (MPXV), which causes mpox clinical disease. Clade I is endemic in Central Africa and can cause severe illness. Clade II, endemic in West Africa, caused the global mpox outbreak that began in 2022 and tends to result in milder illness. Each clade has two known subtypes referred to as “a” and “b.” Clade Ia has been identified in RoC and DRC intermittently for decades and Clade Ib was first identified during the active DRC outbreak. Mpox is a zoonotic disease, meaning it can be spread between animals and people. MPXV has been detected in rodents that live in areas historically affected by mpox.
Genetic sequencing of MPXV can help determine the transmission dynamics and guide the public health response to mpox, but until recently most sequencing of MPXV was done outside of affected countries like RoC, requiring costly sample transport and delaying decision-making by local health authorities.
To better understand whether mpox in RoC was driven by spillover from local animal hosts or cross-border human-to-human transmission from DRC, a team led by the RoC LNSP analyzed 31 samples of laboratory-confirmed MPXV collected through the country’s routine epidemiologic surveillance system between January and April of 2024. Using new in-country sequencing technology, the team determined that there were diverse circulating strains of MPXV in the country, all of the Clade Ia subtype, and some showed up to 99.9% genetic similarity to MPXV sequenced from the DRC. Moreover, MPXV samples came from provinces without historical reports of mpox.
According to the authors, the diversity of identified stains suggest MPXV has been introduced to the human population in RoC through multiple distinct events, which could be a combination of direct zoonotic transmission from local animals as well as human-to-human transmission within and across the country’s borders. They state that current epidemiological data are insufficient to definitively confirm the directionality of MPXV transmission and that further epidemiological research is needed to understand local transmission patterns and inform the public health response in RoC. Finally, they highlight that while only 31 samples met criteria for analysis in the study, it is likely these cases represent only a fraction of the RoC mpox burden at the time of collection.
This research informed the RoC’s decision to declare a national mpox epidemic in April 2024. It is part of a longstanding scientific collaboration between NIAID’s Rocky Mountain Laboratories and the Congolese government. The U.S. Embassy in RoC, the U.S. Agency for International Development, the U.S. Centers for Disease Control and Prevention, and the World Health Organization also provided technical and laboratory support for this study.
Learn more about NIAID’s mpox research priorities. Play a video of NIAID Director Jeanne Marrazzo discussing these priorities.
Reference:
CK Yinda, et al. Genetic sequencing analysis of monkeypox virus clade I in Republic of the Congo: a cross-sectional, descriptive study. The Lancet DOI: 10.1016/S0140-6736(24)02188-3 (2024)