A drug that blocks danger signals that can lead to harmful inflammation could help reduce COVID-19 lung damage, a new study from NIAID scientists and colleagues has found. Scientists from NIAID’s Rocky Mountain Laboratories in Hamilton, Montana, and the University of Utah completed the project, published online in JCI Insights.
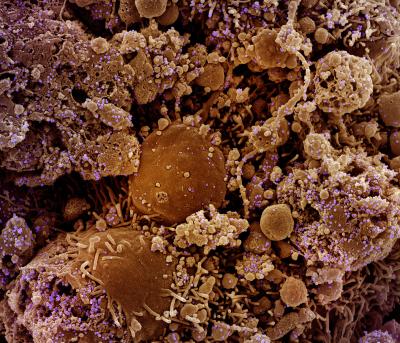
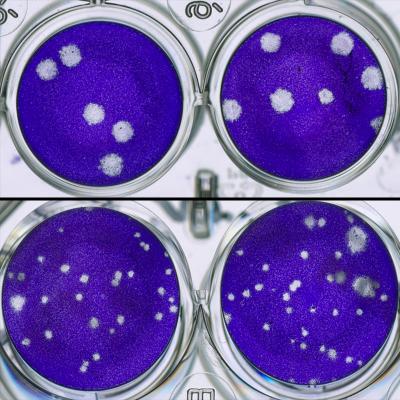
Though they completed the study in laboratory mice modified to model COVID-19 in people, the scientists think their findings are important enough to pursue further studies of the drug, FPS-ZM1, to determine dosing and timing strategies for possible human clinical trials. FPS-ZM1 is an immune modulatory therapeutic – the drug is designed to prevent a specific immune system response from occurring. The investigational therapy has been evaluated in preclinical studies to treat conditions such as diabetes, lung injury and stroke. In their study, the scientists used FPS-ZM1 to block the “receptor for advanced glycation end products” (RAGE), which senses danger signals and can generate inflammation and coagulation known to damage the lungs of COVID-19 patients.
Therapeutic treatment with FPS-ZM1 during the study improved survival in mice infected with SARS-CoV-2, the virus that causes COVID-19. Further, FPS-ZM1 specifically reduced damage to the lung vasculature, an important system for circulating blood through the lungs that becomes damaged during SARS-CoV-2 infection. FPS-ZM1 also has shown in other rodent studies that it can protect against injury in disease models of brain injury, sepsis, asthma, diabetes, acute lung injury and ischemic/reperfusion (organ damage due to blood flow).
The study also identified two distinct phases of COVID-19 disease development in the mice. The scientists want to further explore those phases as potential guides for treatment strategies. For example, FPS-ZM1 limited specific types of inflammation and tissue damage, so it would likely be most effective if administered during the intermediate to later stages of SARS-CoV-2 infection, whereas antiviral treatment may be most effective when given early following infection.
Reference: F Jessop, et al. Impairing RAGE signaling promotes survival and limits disease pathogenesis following SARS-CoV-2 infection. JCI Insights DOI: https://doi.org/10.1172/jci.insight.155896. (2022).