Research
Research Areas
Grants & Contracts
Clinical Trials
News & Events
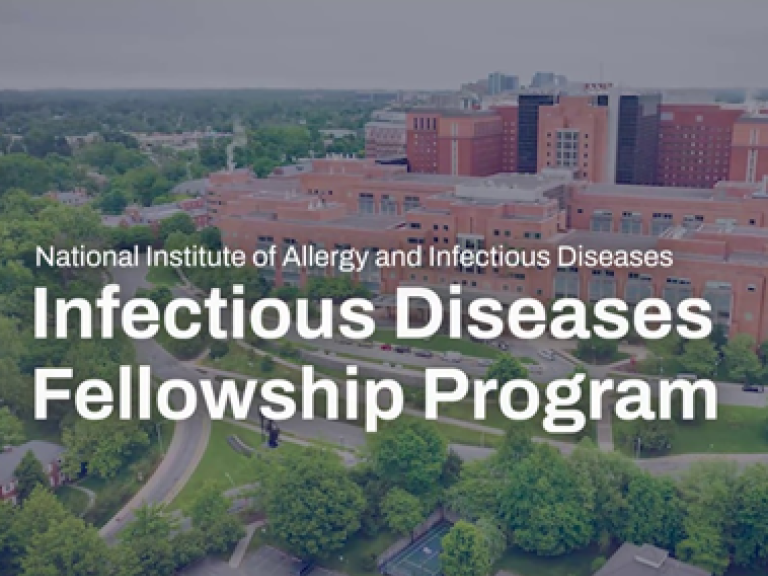
About NIAID
Website Policies and Notices