NIAID’s Division of Microbiology and Infectious Diseases (DMID) is soliciting proposals as part of the 2026 NIAID Omnibus Broad Agency Announcement (BAA). DMID will use this BAA to advance the research and development of promising candidate therapeutics, vaccines, and diagnostics for biodefense and emerging infectious diseases.
The 2026 BAA covers two distinct Research Areas: 001 and 002. Applicants may respond to either one or both Research Areas. See descriptions of each below. For each research area and topic, if applicable, make sure to submit separate technical and business proposals designed to meet the objectives described.
For both research areas:
Performance Period: Not to exceed 5 years (base plus options).
Proposal Submission: Online through the electronic Contract Proposal Submission (eCPS) website.
Research Area 001 – Development of Candidate Therapeutics, Vaccines, and In Vitro Diagnostics for Antimicrobial-Resistant (AMR) Bacterial or Fungal Pathogens
Description: For Research Area 001, there are three separate topics. Offerors may submit a proposal in response to Topics A, B, and/or C:
Topic A: Therapeutics for AMR Bacterial or Fungal Pathogens
The objective of Topic A is to develop new therapeutic products against severe infections and/or drug-resistant strains of the following bacterial and fungal pathogens:
a. Pseudomonas aeruginosa, and/or Acinetobacter baumannii; OR
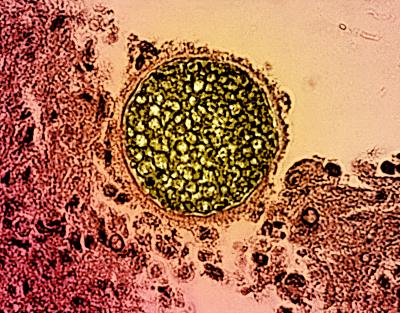
b. Candida auris, Cryptococcus spp., Aspergillus fumigatus, and/or Mucorales
Topic B: Vaccines for AMR Bacterial Pathogens
The objective of Topic B is to protect human health and well-being by advancing vaccine candidates for the following ESKAPE bacterial pathogens: Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species.
Topic C: In Vitro Diagnostics for AMR Fungal Pathogens
The objective of Topic C is to develop innovative platform technologies to speed the identification of infection from among a broad panel of fungi and to profile the phenotypic antifungal susceptibility. This emphasis aligns with NIAID’s goal of addressing persistent challenges in adequate clinical management associated with mycological infections and alleviating the burden of antifungal resistance.
Research Area 002 – Development of Direct Acting Antivirals (DAA) for Viral Families of Pandemic Potential
Description: This Research Area aims to develop safe and effective antivirals to combat viruses of pandemic potential, as well as to build sustainable platforms for targeted drug discovery and the development of a robust pipeline of candidates. Proposals submitted as part of this research area must focus on antivirals that:
- Directly modify viral target function (not through the modulation of the host responses); AND
- Act by reducing viral burden in early stages of disease; AND
- Act against viruses of pandemic potential (i.e., Bunyaviridae, Coronaviridae, Filoviridae, Flaviviridae, Orthopoxviridae, Paramyxoviridae, Picornaviridae, and Togaviridae); AND
- Are new chemical entities limited to small molecules (e.g., natural products, nucleosides, or peptides of </= 40 amino acids) and nanobody conjugates/fusion products that are directly acting on viral targets and functions (not through the modulation of the host responses); AND
- Have safety profiles and suitable routes of administration for broad outpatient use.
Number of Awards, Total Cost: NIAID estimates that one or two awards may be issued for Research Area 001 for a total cost of up to $8.5 million for the non-severable base period across all contracts (direct and indirect costs combined). Three to four awards may be issued for Research Area 002 for a total cost of up to $20 million for the non-severable base period across all contracts (direct and indirect costs combined).
Due Dates: for Research Area 001, February 21, 2025, by 3 p.m. Eastern Time; for Research Area 002, January 21, 2025, by 3 p.m. Eastern Time.
Find complete details in the solicitation itself as well as any amendments issued since this article was published. Direct inquiries to Swee L. Teo, Contracting Officer, at teosl@niaid.nih.gov or 240-669-5173.