This blog is the fourth in a series about the future of NIAID's HIV clinical research enterprise. For more information, please visit the HIV Clinical Research Enterprise page.
The development of HIV therapy is one of the great success stories in modern infectious disease research, marked by rapid advances that scientists in the field could only dream of in the 1980s and 1990s. Once a handful of daily pills that only partially suppressed the virus and caused systemic adverse events, today’s antiretroviral therapy (ART) consists of highly effective, well-tolerated medications that can be taken in a single daily dose or a long-acting injection. ART not only offers individual benefits, but also suppresses viral replication to prevent onward transmission. The understanding that undetectable = untransmittable, also known as “U=U,” is based on the foundational NIAID-funded discovery that an undetectable HIV viral load makes it impossible to transmit the virus to sexual partners.
Today’s high standard of HIV care is possible because of the enduring effort of advocates and policymakers who insist that HIV science be sufficiently funded to address key evidence gaps and public health needs, as well as the research teams that propel a constant stream of discovery and the clinical trial participants who allow their lived experience to become evidence for a population-level benefit. This progress is extraordinary, but more advances are still needed to assure the long-term health and quality of life of all people with HIV. Among many persisting challenges, we must address HIV-related complications and conditions that share health determinants with HIV, including tuberculosis (TB), viral hepatitis and mpox.
NIAID supports four research networks as part of its HIV clinical research enterprise. Every seven years, the Institute engages research partners, community representatives, and other public health stakeholders in a multidisciplinary evaluation of network progress toward short- and long-term scientific goals. This process takes stock of knowledge gained since the networks were last awarded and identifies essential course corrections based on the latest laboratory and clinical evidence. Subsequent NIAID HIV research investments build on the conclusions of these discussions.
These investments are paying off. Recent scientific advances include:
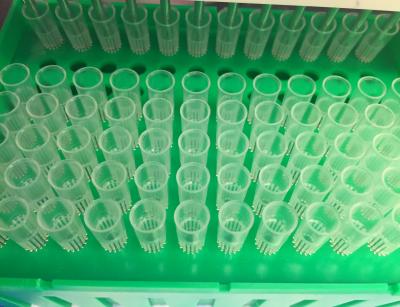
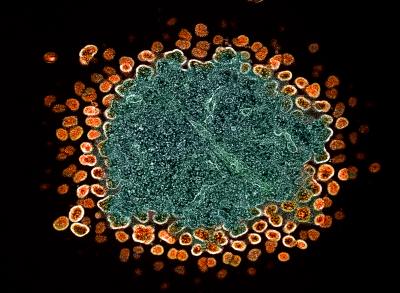
- Basic and translational research that illuminated HIV’s structure, contributing to the development of the first drug in the capsid inhibitor class of antiretroviral drugs;
- A U.S. clinical trial showing that long-acting injectable ART can support viral suppression in people who experience barriers to daily pill-taking;
- A global trial that found daily statin use reduces the risk of major adverse cardiovascular events in people with HIV;
- A large international clinical trial that found a one-month course of rifapentine and isoniazid was as safe and effective as a nine-month course of isoniazid for preventing active tuberculosis in people with HIV;
- Promising results from a hepatitis B virus (HBV) vaccine candidate for people with HIV who do not mount an immune response to current HBV vaccines;
- Evidence that sustained virological response to direct-acting antiviral therapy for hepatitis C virus (HCV) is possible with minimal clinical monitoring—a strategy that could be crucial to the global HCV elimination agenda; and
- Rapid engagement by the ACTG clinical trials network to examine antivirals for COVID-19 and mpox, demonstrating the essential role networks can—and should—play in pandemic preparedness and response.
We look forward to continuing to address the barriers that separate us from truly optimized HIV care. Our goals include fostering the next generation of discoveries that will open up possibilities for people with HIV—including people who have taken ART for decades—to experience a typical lifespan with high life quality, free from a chronic medication burden; reducing the incidence of concurrent TB and hepatitis; and ensuring scientific advances can feasibly be scaled to all who stand to benefit.
Beyond Lifelong ART
Current therapeutic regimens are suppressive at best, meaning that if a person experiences an interruption in treatment, HIV replication will typically resume and continue to damage the immune system. Long-acting formulations are transforming quality of life for people who could not take daily ART, but their durability is measured in months, not years. While substantially extending the durability of ART is feasible, we will reach the limit of what long-acting molecules can do. Beyond the horizon of ART, we are exploring several strategies including gene therapy, administration of broadly neutralizing antibodies, and therapeutic vaccines that could either halt HIV replication for years or life or clear all HIV from the body—efforts collectively grouped under cure research. The design and development of cure strategies must advance technologies that could be implemented at scale, especially in resource-limited settings where HIV prevalence is high.
Non-HIV Pathogens
Even when HIV replication is well-controlled with current therapy, the residual effects of infection can hamper a person’s immune responses and increase their likelihood of experiencing clinical disease from other pathogens. Several infectious diseases also share health determinants with HIV, and require researchers to consider the full constellation of biological, social, and structural factors that can threaten the health of people with HIV. Through collaboration with NIAID’s Division of Microbiology and Infectious Diseases and other NIH Institutes and Centers, we will ensure that we avoid resolving one health condition at the expense of another. We also need to ensure that interventions for non-HIV health conditions will work for people with HIV. Scientific priorities include developing shorter, safer, and more effective treatment regimens for all forms of TB, a preventive TB vaccine, and a hepatitis B cure.
Quality of life
Conditions associated with aging can have greater impact on people with HIV, including (but not limited to) cardiovascular disease, diabetes, perimenopause, and dementia. HIV care models and tools are no longer sufficient if they only support viral suppression. Critical research is underway to define the ways that treated HIV exacerbates or accelerates other chronic conditions seen in older people. In partnership with other NIH Institutes and Centers, we will continue working to improve the quality of life for people with HIV by supporting research to prevent and treat HIV-related coinfections, complications and comorbidities through the lifespan. Furthermore, we will ensure that person-centered HIV care incorporates health-related quality of life metrics alongside standard HIV monitoring and management in our clinical trials.
Equitable progress
Equity remains central to NIAID’s research and development decision-making. ART, once in short supply, is now globally available to most people living with HIV, and long-acting formulations herald a future of easier adherence schedules without the constant reminder of the burden of HIV. While our science has always focused on prioritizing concepts that could be rolled out to all populations who could benefit, we must provide an evidence base to support a faster translation of discovery to equitable health care service delivery. Implementation science and social science research including behavioral research, together with medical advances, can accelerate progress toward health equity. We seek to maintain a continuous feedback channel with implementers, so that our priorities are aligned with their most pressing challenges.
The research community plays an essential role in shaping NIAID’s scientific direction and research enterprise operations. We want to hear from you. Please share your questions and comments at NextNIAIDHIVNetworks@mail.nih.gov.
About NIAID’s HIV Clinical Trials Networks
Advancing Clinical Therapeutics Globally for HIV/AIDS and Other Infections is a global clinical trials network that conducts research to improve the management of HIV and its comorbidities; develop a cure for HIV; and innovate treatments for tuberculosis, hepatitis B, and emerging infectious diseases. The Network is supported through grants from NIAID, with co-funding and scientific partnership from the NIH National Institute of Mental Health, the NIH National Institute on Drug Abuse, the NIH National Institute on Aging, and other NIH Institutes and centers. Three other networks—the HIV Vaccine Trials Network, the HIV Prevention Trials Network, and the International Maternal Pediatric Adolescent AIDS Clinical Trials Network—generate complementary evidence on the scientific areas within their respective scopes.