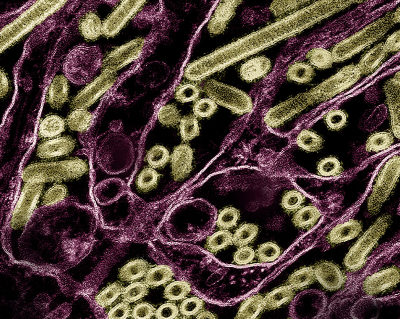
An experimental vaccine designed against the highly pathogenic avian influenza H5N1 (HPAI H5N1) virus circulating in U.S. cattle was fully protective in research mice in a new study published in Nature Communications. NIAID scientists at Rocky Mountain Laboratories (RML) in Hamilton, Montana, led the animal study with colleagues from HDT Bio in Seattle who developed the replicating RNA vaccine (repRNA) platform.
Along with confirming that a single immunization with the experimental vaccine was effective against the new flu type in cattle (HPAI A H5N1 clade 2.3.4.4b), the study also allowed scientists to evaluate the vaccine method for “cross protection.” Would it work against the new virus if designed with components used in stockpiled vaccines from an older H5N1 virus (A/Vietnam/1203/2004)? They found that when the test vaccine used a design from the older H5N1 virus, protection was diminished. The findings suggest that the HPAI H5N1 circulating in the U.S. may be able to evade immunity from older H5N1 viruses.
Scientists designed the repRNA vaccine to express the protective vaccine components, as well as the RNA replication machinery derived from an alphavirus. This allows for robust expression of the protective vaccine components upon delivery with LION™, a proprietary nanoparticle formulation. The repRNA/LION technology is the basis of a vaccine that received emergency use authorization in India for COVID-19. Additional applications of repRNA/LION are advancing toward clinical trials for other serious viral diseases after showing effectiveness against several different viruses in the lab.
Scientists at RML and HDT Bio are continuing to develop the vaccine platform, and evaluations in animal models developed at RML are ongoing.
Reference: D Hawman, et al. Clade 2.3.4.4b but not historical clade 1 HA replicating RNA vaccine protects against bovine H5N1 challenge in mice. Nature Communications DOI: https://doi.org/10.1038/s41467-024-55546-7 (2025).