Calling for Reinforcements: A New Way to Recruit Immune System Helpers Could Lead to Better Flu Vaccines
Each year, flu causes hundreds of thousands of deaths and millions of hospitalizations worldwide. Although the best way to protect against serious illness is annual vaccination, the influenza vaccine’s effectiveness is far from perfect. In the past decade, CDC estimates of flu vaccine effectiveness have ranged from a low of 19% to a high of 48%, spurring calls for development of more effective flu vaccines. Now, NIH-funded researchers at the Stanford University School of Medicine have taken a new approach to crafting flu vaccines that resulted, both in mice and human tonsil tissue, in a more broadly protective immune response compared to currently available flu vaccines. The studies were led by Mark M. Davis, Ph.D., and the findings appeared in Science.
The trouble with current vaccines
Currently, flu vaccines are formulated annually to contain up to four strains of human influenza virus that are predicted to circulate widely in the coming season. For example, the 2024-2025 seasonal flu vaccine contains two strains of the influenza viurs A subtype and one of influenza virus B subtype. Each virus strain includes a viral protein called hemagglutinin (HA) that the virus uses to attach to and enter human cells. The immune system recognizes and responds to components of a virus or a vaccine—the antigens—by generating protective antibodies and T cells. On exposure to the flu virus, a subset of flu-specific T cells, called CD4+ helper T cells, provides signals to generate and activate antibody-producing B cells. Ideally, a swarm of HA-matched antibodies is produced following vaccination and will protect the vaccinated person from infection by flu virus strains represented in that year’s vaccine. However, each person tends to make a strong response to only one or a few of the vaccine HAs, leaving them vulnerable to other flu virus strains they may encounter. This phenomenon is known as subtype bias.
Original antigenic sin
Subtype bias has long been explained using the evocative term “original antigenic sin.” It holds that the first influenza antigen a person is exposed to skews all future antibody and T cell responses towards that antigen. If original antigenic sin correctly explains subtype bias, then the outlook for improved, broadly protective flu vaccines is dimmed. But what if that explanation does not accurately account for subtype bias? Then perhaps there might be ways to overcome it. Dr. Davis and his colleagues set out to see if this was possible.
The investigators first looked at patterns of subtype bias in two groups of study participants: 78 identical twins and 15 very young “influenza naïve” infants (who repeatedly tested negative for flu exposure during the study). Among the twins, 77% displayed bias for one flu subtype. That is, they preferentially made strong antibody responses to just one flu subtype in the vaccine, in preference to the others. The same preference for one subtype over the other three was seen in 73% of the influenza-naïve infants, suggesting that an individual’s genetic make-up likely plays a bigger role in driving subtype bias, although initial virus exposure also has some effect.
Overcoming bias and calling in more helpers
Can subtype bias be overcome? The team explored that question in their effort to get B cells to make antibodies against all the HAs included in seasonal flu vaccines. Instead of using a mixture of four separate flu virus strains (each possessing a different HA antigen) as is the case in standard flu vaccines, Dr. Davis and colleagues synthesized a small molecule consisting of a single scaffold backbone to which all four HAs were then attached, forming a multi-antigen construct containing equal amounts of each HA protein.
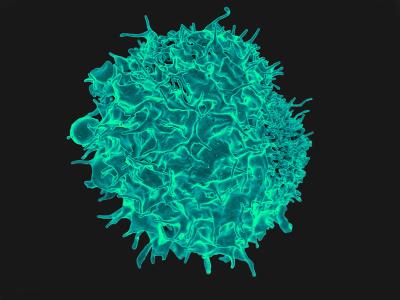
These heterologous HA antigen constructs are small enough to be taken up by B cells, which then digest the HAs and display small pieces of them on the cell’s surface where it draws the attention of CD4+ helper T cells. These helper cells aid in turning the B cell from an antigen-displaying cell to an antibody-producing cell. Ordinarily, a B cell will ingest and display pieces of just one HA antigen and get assistance from only a subset of helper T cells. In contrast, Dr. Davis and his colleagues found that when a B cell ingests the coupled heterologous HA construct, it displays components of all four HA antigens and can engage a wider population of helper T cells. Those helper T cells can interact with a wider range of B cells leading to production of more antibodies against all four HA antigens.
Dr. Davis’s team then conducted a study in mice showing that the heterologous four HA antigen vaccine limited the subtype bias that prevailed when animals were immunized with a flu vaccine made in the standard way.
Tonsil tissue
The investigators next tested the four-antigen coupled heterologous HA construct in human tonsil tissue obtained from tonsillectomy surgeries. They processed the raw tissue into small fragments that in culture dishes form multicellular structures called organoids. These organoids have structural features and functional capabilities similar to tonsils, lymph nodes, and other lymphatic tissues where T and B cells interact. When exposed to either standard inactivated seasonal influenza vaccine or to a mixture of HA antigens, B cells in the tonsil organoids produced antibodies in a subtype-biased manner. However, cultured organoids that were stimulated with the heterologous four HA antigen constructs produced higher antibody responses against multiple flu subtypes. The organoids also generated more activated CD4+ helper T cells when stimulated with the coupled HA antigen construct relative to that seen with standard inactivated influenza vaccine.
From these experiments, the scientists concluded that, “coupling heterologous antigens may broaden T cell help and improve vaccine efficacy. This strategy to augment T cell help is readily applicable to vaccines for other pathogens where multi-strain coverage is needed.”
Reference: V Mallajosyula et al. Coupling antigens from multiple subtypes of influenza can broaden antibody and T cell response. Science. DOI: 10.1126/science.adi2396 (2024).