With cholera importation again a looming threat to America, Kinyoun entered the Marine-Hospital Service (MHS) on 4 October 1886 (Figure 9) (11, 25, 27) in a key position at the Staten Island quarantine station, the most likely port of entry for exportable European infectious diseases like cholera. The life of an MHS officer in this era was typically one of adventure but also of danger, with many officers dying in the line of duty, especially from yellow fever and other infections they were trying to contain. As was customary in the MHS, and probably as a legacy of the secretive former military man/MHS Surgeon General Woodworth (11), Kinyoun received a code name he carried with him throughout his MHS career: Abutment. The New York quarantine station hospital (still standing as of 2012) was a facility newly rented from the Marine Society (Figures 10–14) (28–33), the entire station having just been relocated from Bedlow (Bedloe) Island (now called Liberty Island) to allow construction there of the Statue of Liberty. Hamilton quickly set up the nation’s first federal bacteriology laboratory in a museum room and placed the 26-year-old newcomer in charge of it (2, 28, 29). Kinyoun opened up shop in August 1887 (2, 28, 29)—apparently on August 27 (33), the beginning of the NIH.
Kinyoun’s 16-year MHS career corresponded with the emergence and growth of American microbiology and epidemiology and an MHS-influenced expansion of national public health. The Hygienic Laboratory began as a diagnostic laboratory supporting MHS quarantine activities against the (then) four quarantinable epidemic diseases: cholera, yellow fever, smallpox, and plague. At the time, cholera and yellow fever were the biggest of these threats; cholera was potentially the most amenable to new approaches due to Koch’s 1884 isolation of a putative causative organism (24), which allowed for patient diagnosis and environmental detection using bacteriologic techniques. Especially during the warm weather “quarantine season,” American consular offices around the world would cable the MHS about outbound ships that might harbor any of these quarantinable diseases, or which had left ports with ongoing epidemics. MHS officers in U.S. ports would then meet and inspect the ships, examine patients, conduct epidemiological investigations and, if necessary, quarantine and fumigate the ships, cargo, and ballast while disinfecting and isolating ill and well passengers, clothes, possessions, and mail (34).
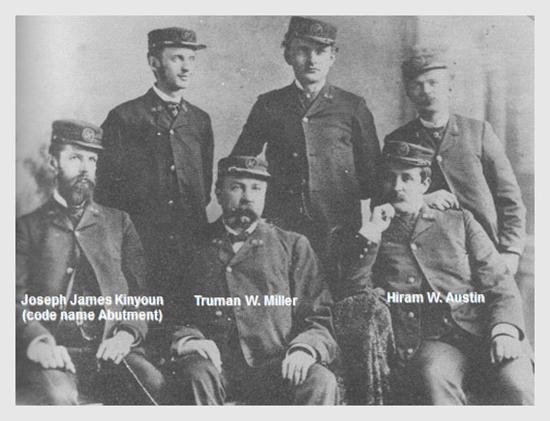
Figure 9. Joe Kinyoun joined the Marine-Hospital Service in 1886 as an Assistant Surgeon assigned to the Staten Island, New York, quarantine station. The time and circumstances of this photograph are unknown, but can be provisionally dated to late 1886 because Kinyoun (front row, left; still bearded as he had been in earlier years) joined the MHS around the time that Truman W. Miller (1840–1900; front row, center) resigned his commission. Miller later became editor of The Journal of the American Medical Association following the death of its previous editor, former MHS Surgeon General John B. Hamilton. The Journal supported Kinyoun throughout his career. On Miller’s left is MHS Officer Hiram W. Austin (1850–1932). The other MHS officers have not been conclusively identified. It is noteworthy that Kinyoun, a sophisticated amateur photographer with his own darkroom, is holding the camera flash tripwire in his left hand. Kinyoun took other such portraits and professional quality photographs over the years, often carried a camera around in his pocket, and gave his wife Lizzie the “camera craze” (as he termed it) to the point where she regularly stayed up nights developing and printing photographs (11). He may also have influenced his father to take up the hobby, as suggested by a formal self-portrait in which John Hendricks Kinyoun holds the camera tripwire in his left hand. The above photograph has previously been published but with apparently incomplete and erroneous identifying information (25, 27)

Figure 10. The (eastward facing) front of the Marine Hospital, Stapleton, Staten Island, New York, which housed the Hygienic Laboratory from 1887–1891 (27–29). In 1891 the laboratory moved to Washington, DC, leaving behind a smaller service laboratory. The building still stands (as of 2012) but is unoccupied (Figure 11). The exact location of the laboratory is unknown, but it was in one of the eight apparently identical ground floor rooms in the central part of the building. The windows of four of those rooms are visible above, two on either side of the main entrance. Four additional central ground floor rooms are in the back of the building (see Figure 12). The two men are unidentified but are presumably Marine-Hospital Service officers. It has been speculated that Kinyoun is on the left and station director (later Surgeon General) Walter Wyman is on the right.
Figure 11.The former MHS hospital on Errington Street, Stapleton, Staten Island, New York, now abandoned, as seen from above. The eastward facing front of the hospital is visible in the lower part of the picture. Google satellite photograph, 2010.
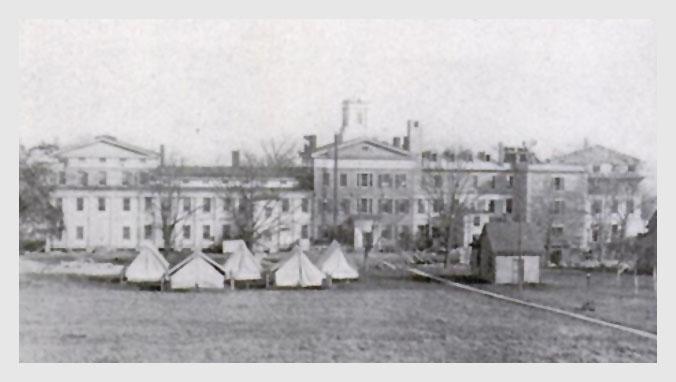
Figure 12. The (west facing) rear of the Marine Hospital, Stapleton, Staten Island, New York, where the Hygienic Laboratory was located from 1887–1891. Isolation tents for tuberculosis patients are visible behind the building. Kinyoun instituted this tuberculosis isolation, apparently being among the first to do so, and he urged unsuccessfully that other Marine Hospitals follow suit (31, 32).
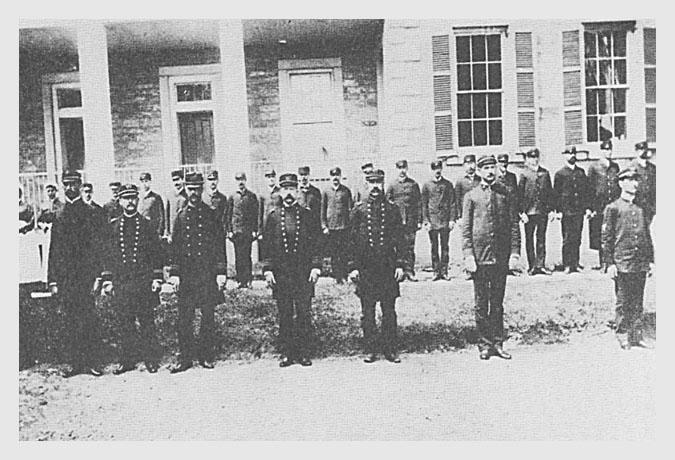
Figure 13. MHS officers (front row, second through fifth men) and other employees, (e.g., stewards, dock workers, and clerks) (first row, first and last two men; all of back row), posed in front of the southern part of the east wing, Marine Hospital, Stapleton, Staten Island, New York, 1887. Kinyoun stands third from the left; Walter Wyman stands to his left (i.e., center). The other men have not been conclusively identified.
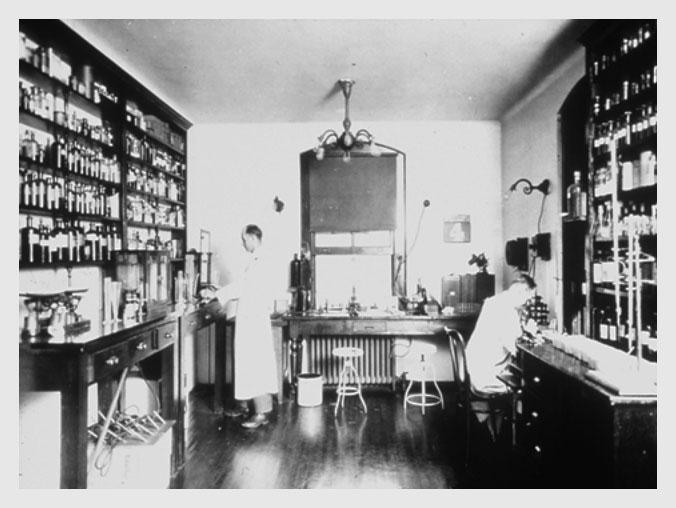
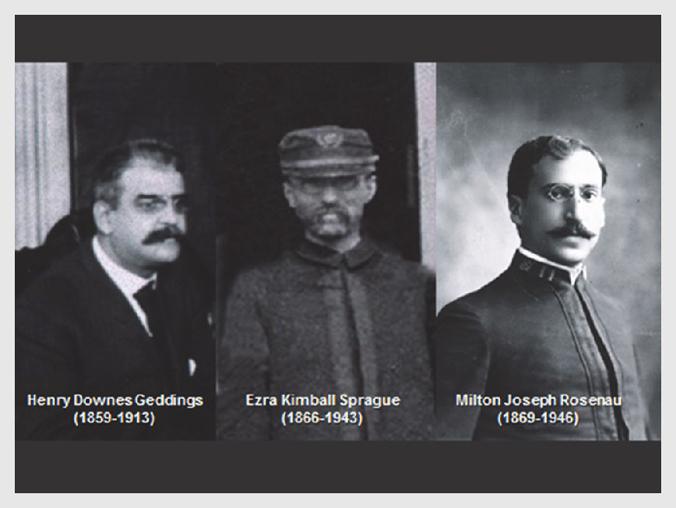
Figure 14. The original Hygienic Laboratory on the first floor of the main building of the rented Marine Hospital, Stapleton, Staten Island, New York. The image is undated but was presumably taken between 1887 and 1891. The building is still standing, but is unoccupied (Figure 11). The actual location of this room, in one of eight similar rooms on the ground floor of the central building, is not currently known. The Hygienic Laboratory moved to the 4th floor of the Butler Mansion, adjacent to the U.S. Capitol, in 1891. The two men in the picture have not been identified but neither appears to be Kinyoun, or Wyman, or any of the other early Hygienic Laboratory supervisors, such as Henry Downes Geddings (1859–1913), Ezra Kimball Sprague (1866–1943), or Milton Joseph Rosenau (1869–1946).
Kinyoun had barely set up the Hygienic Laboratory when an Italian ship arrived in New York on 22 September 1887, reporting eight suspected cholera deaths en route; a sister ship followed shortly thereafter with three more deaths en route. Cholera had never been isolated in the United States; indeed, there were only a handful of men who had the knowledge and equipment to do so. Kinyoun’s investigation led him to obtain cultures from living and (later) dead autopsied cholera patients that grew cholera vibrios, work which was thereafter confirmed by his friends Edward Orem Shakespeare (1846–1900; Blockley Hospital, Philadelphia), Biggs (at Bellevue), and T[heophil] Mitchell Prudden (1849–1924; at the [New York] College of Physicians and Surgeons) (Figure 6), to whom he had sent the cultures for “blind” confirmation. Only when the three men met to compare results—all positive—did Kinyoun and his Missouri MHS colleague Samuel Treat Armstrong (1859–1899) report the sensational news of the first bacterial detection of cholera in the Western Hemisphere (35,36). With the coup he had hoped for, Hamilton began boasting about Kinyoun and the Hygienic Laboratory, while gradually expanding its scope. As these events were unfolding, Kinyoun’s 3-year-old daughter Bettie contracted and died of diphtheria (18), her physician father unable to save her. Diphtheria was the same terrible disease that had killed Kinyoun’s New York patient and brought him close to quitting medicine forever. Bettie’s death was a tragedy from which Kinyoun would never fully recover. He poured himself into work. The MHS soon overcame the National Board of Health to survive as the nation’s sole public health agency (2). Within two years, in 1889, The Journal of the American Medical Association was calling for a “United States Public Health Service,” an idea and a term still more than two decades away from realization. Even before authorizing legislation was enacted by Congress, Kinyoun moved beyond pure bacteriologic support of quarantine measures, extending his research to other infectious diseases of public health importance.
From 1887 until he stepped down as Hygienic Laboratory director 12 years later, Kinyoun pushed himself and the laboratory rapidly forward as mostly European microbiology breakthroughs created ever more applied research opportunities. He was fully supported by Hamilton and by Hamilton’s successor Walter Wyman (1848–1911) (Figure 15) (37), another officer who had once studied in European laboratories in the pre-microbiology era.

Figure 15. MHS officer Walter Wyman (1848–1911) served as Surgeon General from 1891 until his death from complications of diabetes in 1911. Kinyoun had been a protégé of prior Surgeon General Hamilton and was already a rising star in the MHS when Wyman, his supervisor at the New York quarantine station, became Surgeon General. The nature of the relationship between Kinyoun and Wyman has been a source of speculation for over a century. There is substantial evidence both for and against the notion that Wyman was unsupportive of Kinyoun although, as a militaristic “by the books” manager, if he had felt any ill will toward Kinyoun, Wyman would probably never have openly displayed it. Although Kinyoun never challenged Wyman’s authority, Wyman may have felt threatened by Kinyoun’s substantial national/international reputation. The Journal of the American Medical Association, run for a time by Wyman’s enemy and former MHS Surgeon General Hamilton, repeatedly praised Kinyoun and disparaged Wyman. For example, a Journal editorial called Wyman unfit for his job and another referred to Kinyoun as “Surgeon General Kinyoun.” The two men worked closely together, with Wyman being Kinyoun’s immediate supervisor throughout Kinyoun’s entire 16-year MHS career. During almost the entire period, he seems to have been Wyman’s principal “go to” man; they appear never to have had any official dispute, although Kinyoun claimed that after his MHS resignation, he told Wyman he had a low opinion of his leadership (37).
In 1888, the New Orleans quarantine station was reorganized according to Kinyoun’s recommendations, setting the stage for important yellow fever studies of the next decade (38). In late 1888, Kinyoun took an additional three months of laboratory training at Johns Hopkins under Welch (36). Later that year, Kinyoun’s first MHS protégé, Henry Downes Geddings (1859–1913), began running a spinoff yellow fever laboratory in Florida’s Dry Tortugas (Figure 16). When Robert Koch (1843–1910) announced that tuberculin was a cure for tuberculosis in 1890 (39–41), Kinyoun went to Berlin as a visiting scientist—simultaneously chaperoning the family of Lizzie’s cousin, Georgia Sen. Joseph E. Brown (1821–1894)—and became among the first to conclude, based on laboratory and hospital investigations under Koch’s direct supervision and at the Charité and Maobit hospitals, that tuberculin was not the hoped for cure (39, 40). Even so, he helped his German colleagues better evaluate treatment efficacy with modification of clinical study methods to introduce standardized examinations of patients, thereby controlling for type and severity of disease in those who did and did not receive treatment (39, 40).
As he worked in Berlin, Kinyoun sent tuberculin to Geddings with instructions to set up a parallel tuberculin clinical research program in Washington, DC (41). Somehow he managed to retain both his own skepticism about tuberculin and Koch’s friendship, conducting a series of experiments under Koch while simultaneously working with Koch’s most irritating critic, Rudolf Virchow (1821–1902) (Figure 17). From Kitasato Shibasaburō (1853–1931), the Koch laboratory’s fellow visiting scientist from Cambridge, Ernest Hanbury Hankin (1865–1939), and from Paris-based Ilya Mechnikov (1845–1915), Kinyoun learned nascent principles of immunology (40), an even newer field than microbiology. He (correctly) predicted that further breakthroughs were inevitable, “[i]f the [immunological] theories of Kitasato, [von] Behring, and Hankin could be put into practical operation in combating acute infectious diseases by immunizing persons against them . . .” (40). Among the first scientists to fully appreciate the intimate relationship between microbiology and immunology, Kinyoun went on to articulate an early concept of two different components of immunity: innate and acquired immunity. From Berlin, he continued on to Paris to work under Pasteur, learning, among other things, how to produce rabies vaccine.

Bringing reagents, techniques, protocols, and ideas back to the United States, Kinyoun turned the Hygienic Laboratory—which moved to Washington, DC, in 1891 (Figures 18 and 19)—into a modern European style laboratory strongly oriented toward research with applied public health and clinical applications, while simultaneously supporting the many ongoing MHS outbreak investigations (Exhibit 1). Exhibit 1. Kinyoun’s first decade (1887–1896) as director of the Hygienic Laboratory. Selected research projects undertaken by Kinyoun and other efforts, organized by the year begun. In addition to these activities, Kinyoun was responsible for running the Hygienic Laboratory and supporting the investigations and diagnostic needs of the other MHS officers stationed across the country and abroad. Dates are approximate in some cases. See monograph text for additional information and references.
Exhibit 1. Kinyoun’s first decade (1887–1896) as director of the Hygienic Laboratory. Selected research projects undertaken by Kinyoun and other efforts, organized by the year begun. In addition to these activities, Kinyoun was responsible for running the Hygienic Laboratory and supporting the investigations and diagnostic needs of the other MHS officers stationed across the country and abroad. Dates are approximate in some cases. See monograph text for additional information and references.
1887—Studied cholera diagnosis and growth properties in sea water; urged hospital isolation of tuberculosis patients; began work that debunked Carlos Finlay’s claim for a micrococcal etiology of yellow fever but began correspondence with Finlay and was eventually persuaded by Finlay’s theory of mosquito transmission.
1888—Studied microbial disinfection with steam/pressure and later sulfur and formaldehyde; began invention of multiple disinfecting machines.
1889—Studied bacteria on hands, nosocomial transmission by health care workers, and epidemiology of pneumococcal pneumonia and hospital carriage epidemics; identified role of pre-outbreak bacterial colonization in institutional epidemics; developed early credible theory of why pneumococcal epidemics usually occurred in winter.
1890—Studied yellow fever etiology, pandemic influenza, malaria, and lack of efficacy of cobra venom as cholera treatment.
1891—Proved lack of efficacy of tuberculin in treatment of tuberculosis; produced rabies vaccine; prepared first pneumococcal vaccine and first pneumococcal immune serum; studied “enteric fever”; studied contamination of potable water and water safety standards.
1893—Helped prepare new federal quarantine regulations; set up Hygienic Laboratory exhibit at the World's Columbian Exposition ("Chicago World’s Fair").
1894—Was first American to study newly discovered plague bacillus; studied new diphtheria antitoxin in Berlin, Paris, and Washington, DC; became first to prepare and test smallpox immune serum in humans; conducted study of ventilation of U.S. House of Representatives; began three-month laboratory instruction course for MHS officers. Cohosted Convention of American Bacteriologists, first national organization of American microbiologists, followed four years later by the Society of American Bacteriologists (now the American Society for Microbiology); served as President in 1909.
1895—Warned about plague importation to United States; increased outbreak investigations related to general public health and unrelated to quarantine or marine issues; worked on typhoid fever.
1896—Conducted studies to distinguish variola from vaccinia; researched malaria; worked on streptococcal vaccine; began plague research program; worked on disinfection of railway coaches; was active against anti-vivisection movement; taught courses to civilians in Hygienic Laboratory.
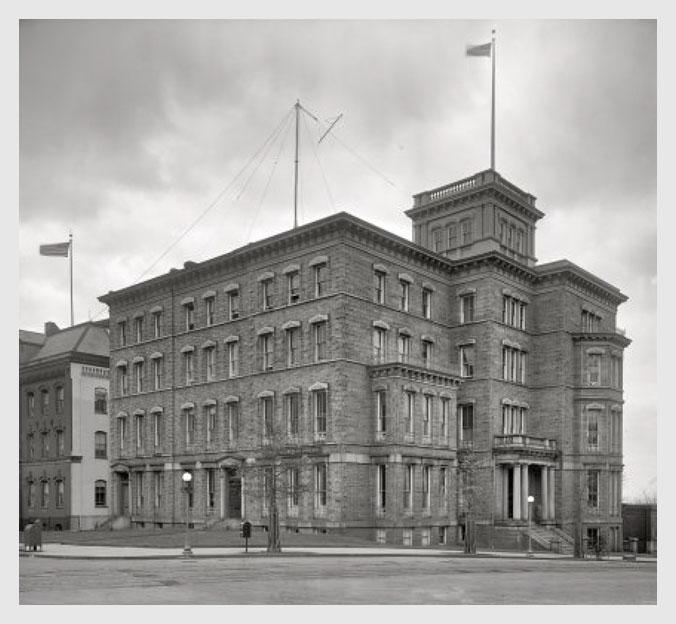
Figure 18.The Butler Mansion, at the corner of B Street and 3rd Street Southeast, Washington, DC. The MHS moved to this building in 1891, and the Hygienic Laboratory occupied the entire 4th (upper) floor. The view from B Street windows looked directly across the street at the South end of the U.S. Capitol. The Butler Mansion had served as a temporary White House during the administration of president Chester A. Arthur (1829–1886), but by 1891 had been converted to office space for the MHS and other federal agencies.
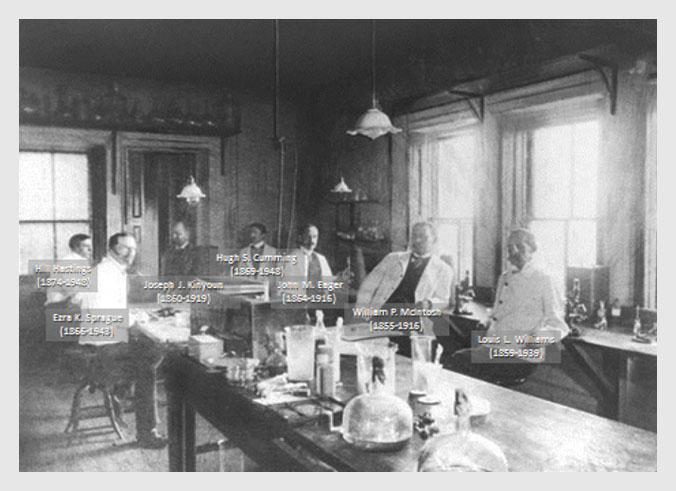
Figure 19. The Hygienic Laboratory in its second home, occupying the4th floor of the Butler Mansion, across the street from the South end of the U.S. Capitol in Washington, DC. The photograph is undated but was presumably taken in early 1899. At the time, Ezra Sprague was Kinyoun’s principal assistant; Hugh S. Cumming (1869–1948) was a new MHS officer training under Kinyoun and later became U.S. Public Health Service Surgeon General. John Macauley Eager (1864–1916) later became Assistant Surgeon General. Louis L. Williams (1859–1939) later became Chief Medical Officer on Ellis Island.
From the outset, he believed that the Hygienic Laboratory “should form the nucleus of one national in its character” (31). In support of quarantine practice, Kinyoun invented numerous industrial disinfecting machines and experimented with temperature and pressure variables in them (42). Returning to Berlin and Paris in 1894, he became the first American to study Kitasato’s/Yersin’s newly discovered plague bacillus, and was also fortunate to witness firsthand a spectacular therapeutic breakthrough that must have had great personal significance: von Behring and Kitasato’s diphtheria antitoxin (43–45). Kinyoun seems to have fully comprehended that he stood at the beginning of “a new epoch” (46). On the hospital wards, in the laboratory, and poring over clinical and epidemiologic information in both Paris and Berlin, he admitted that “I have tried hard to find fault, to pick flaws in the statistics, but have signally failed. The work must stand for itself,” and “[it] has opened up a whole new field in infectious diseases” (43, 44). Perhaps remembering his own lost Bettie, Kinyoun was even moved to perhaps the least guarded comment yet found in his scientific writings and speeches, describing the antitoxin’s lifesaving effect on dying children as “so astounding that at first one is almost compelled to ask one’s self ‘is this possible?’ ” (44, 45).
Back home, Kinyoun set about producing and distributing diphtheria antitoxin and other new biologicals (47), inviting specialists from around the nation to come to the Hygienic Laboratory to take a six-week course in preparation techniques under him, and making diphtheria antitoxin available to all of the MHS hospitals and to private physicians who were willing to send him detailed clinical information about their patients. He pleaded that physicians now had a moral responsibility to correctly diagnose and promptly treat their patients. As the lifesaving antitoxin began to be used, Kinyoun was also keenly interested in its impact on the epidemiology of diphtheria. He concluded that subclinical cases and those treated successfully were still transmitting diphtheria to others. In addition, he found that, although successful treatment was saving lives, it was actually increasing disease transmission, particularly to close contacts, because recovered children were quickly removed from isolation to resume contact with family members and schoolmates. He sent out and tested reagents, consulted with physicians and scientists, and became a committed advocate eager to speak at national and neighborhood meetings on hygiene, public health, and good medical practice. To save as many children as possible, Kinyoun set up a public diphtheria laboratory at Georgetown Medical School, at great personal expense (38).
Kinyoun developed a smallpox immune serum and tested it in a human clinical trial, apparently the first such effort anywhere (48). He kept up an energetic multifaceted research program (Exhibit 1); worked on making a streptococcal vaccine; was among the earliest to develop an experimental pneumococcal vaccine and an immune serum (49); conducted important yellow fever work; studied bacterial carriage and transmission by well carriers; advocated for nosocomial (hospital- and medical-care-acquired) infection control (46); and in his spare time studied the brand new technique of Roentgenology (radiology) while getting a Ph.D. from Georgetown University in 1896. In the early 1890s, he mentored would-be Army researcher Walter Reed, who became a lifelong friend and confidant. When the U.S. House of Representatives requested it, he conducted an investigation of the ventilation of House chambers and suggested cost-effective changes, wryly implying that the offensive odor problem was partly due to members spitting tobacco juice onto the carpet (50). When Teddy Roosevelt and the Rough Riders came back from the Spanish-American war, Kinyoun put them under quarantine in Camp Wickoff, at Montauk Point, Long Island, to be treated for malaria, measles, and enteric fevers (51).
In Kinyoun’s 1897 summary of the Hygienic Laboratory’s first decade, he boldly proposed that instead of merely trying to study and control infectious diseases during epidemics, the federal government should create a laboratory-supported national and international research enterprise to “[look] into the nature, origin, and prevention of contagious epidemics, and other diseases affecting the people, and should also make investigations into other matters relating to public health” (52). This was a farsighted notion that went beyond the visions of most others in anticipating its mandate when it became the NIH some 33 years later. Meanwhile, the Hygienic Laboratory was expanding, and Kinyoun was developing increasingly comprehensive laboratory training programs for MHS officers (53).

