Severe combined immunodeficiency (SCID) is a group of rare disorders caused by mutations in different genes involved in the development and function of infection-fighting immune cells. Infants with SCID appear healthy at birth but are highly susceptible to severe infections. The condition is fatal, usually within the first year or two of life, unless infants receive immune-restoring treatments, such as transplants of blood-forming stem cells, gene therapy, or enzyme therapy. More than 80 percent of SCID infants do not have a family history of the condition. However, development of a newborn screening test has made it possible to detect SCID before symptoms appear, helping ensure that affected infants receive life-saving treatments.
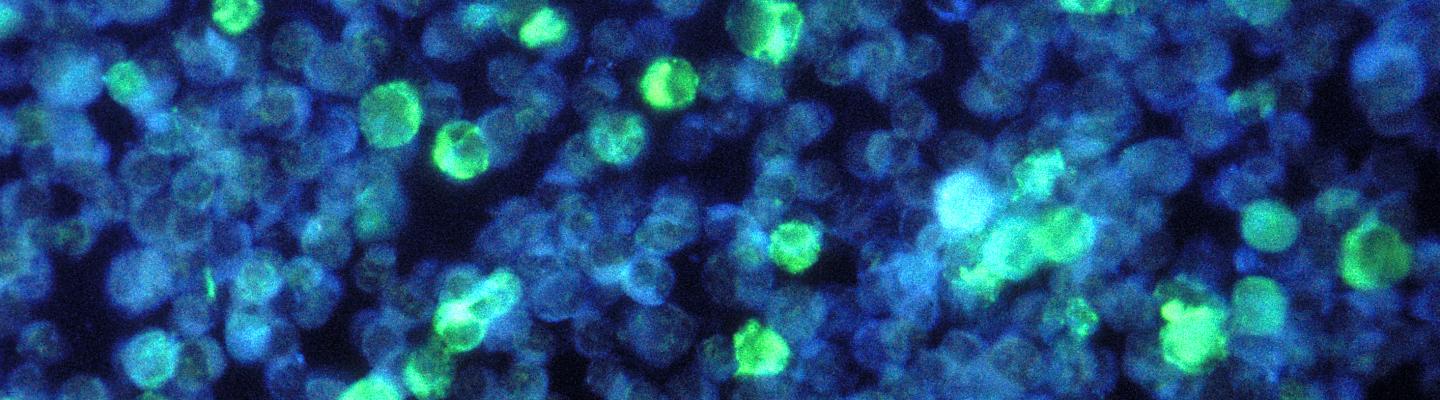
More than a dozen genes have been implicated in SCID, but gene defects are unknown in approximately 15 percent of newborn-screened SCID infants, according to an NIH-funded study. Most often, SCID is inherited in an autosomal recessive pattern, in which both copies of a particular gene—one inherited from the mother and one from the father—contain defects. The best-known form of autosomal recessive SCID is caused by adenosine deaminase (ADA) deficiency, in which infants lack the ADA enzyme necessary for T-cell survival. X-linked SCID, which is caused by mutations in a gene on the X chromosome, primarily affects male infants. Boys with this type of SCID have white blood cells that grow and develop abnormally. As a consequence, they have low numbers of T cells and natural killer cells, and their B cells do not function.
Symptoms of SCID occur in infancy and include serious or life-threatening infections, especially viral infections, which may result in pneumonia and chronic diarrhea. Candida (yeast) infections of the mouth and diaper area and pneumonia caused by the fungus Pneumocystis jirovecii also are common.
The SCID newborn screening test, originally developed at NIH, measures T cell receptor excision circles (TRECs), a byproduct of T-cell development. Because infants with SCID have few or no T cells, the absence of TRECs may indicate SCID. To confirm a SCID diagnosis, a doctor will evaluate the numbers and types of T and B cells present and their ability to function. Research supported by NIAID and other organizations has shown that early diagnosis of SCID through newborn screening leads to prompt treatment and high survival rates. SCID was added in 2010 to the U.S. Department of Health and Human Services’ Recommended Uniform Screening Panel for newborns. Today, all newborns in the United States are screened for SCID.
Hematopoietic (blood-forming) stem cell transplantation is the standard treatment for infants with SCID. Ideally, infants with SCID receive stem cells from a sibling who is a close tissue match. Transplants from matched siblings lead to the best restoration of immune function, but if a matched sibling is not available, infants may receive stem cells from a parent or an unrelated donor. These transplants are life-saving, but often only partially restore immunity. NIAID-supported research has shown that early transplantation is critical to achieving the best outcomes for SCID infants. Investigators analyzed data from 240 infants with SCID and found that those who received transplants before the age of 3.5 months were most likely to survive, regardless of the type of stem cell donor used.
Children who have SCID with ADA deficiency have been treated somewhat successfully with enzyme replacement therapy called PEG-ADA.
Studies also have shown that gene therapy can be an effective treatment for some types of SCID, including X-linked SCID. In gene therapy, stem cells are obtained from the patient’s bone marrow, the normal gene is inserted into the stem cells using a carrier known as a vector, and the corrected cells are returned to the patient. Early efforts to treat X-linked SCID with gene therapy successfully restored children’s T-cell function, but approximately one-quarter of the children developed leukemia two to five years after treatment. Scientists suspect that the vectors used in these studies activated genes that control cell growth, contributing to leukemia. Newer gene therapy strategies use modified vectors that appear effective and safe. NIAID researchers are using a novel gene therapy approach to successfully treat older children and young adults with X-linked SCID.
Scientific Advances
Screening Newborns for Deadly Immune Disease Saves Lives
June 20, 2023Introducing widespread screening of newborns for a deadly disease called severe combined immunodeficiency, or SCID, followed by early treatment boosted the five-year survival rate of children with the disorder from 73% before the advent of screening to 87% since, researchers report. Among children whose disease was suspected because of newborn screening rather than illness or family history,…