XLA is an inherited immune disorder caused by an inability to produce B cells or the immunoglobulins (antibodies) that the B cells make. XLA is also called Bruton type agammaglobulinemia, X-linked infantile agammaglobulinemia, and congenital agammaglobulinemia.
Causes
The mutated gene responsible for XLA codes for the protein Bruton tyrosine kinase, or BTK, and is located on the X chromosome, and is an X-linked recessive disease. Because males only have one X chromosome, they are affected if they inherit an X chromosome containing a mutated BTK gene.
Symptoms
Infants with XLA develop frequent infections of the ears, throat, lungs, and sinuses. Serious infections also can develop in the bloodstream, central nervous system, skin, and internal organs. These children tend to cope well with most short-term viral infections but are very susceptible to chronic viral infections such as hepatitis. They usually lack or have very small tonsils.
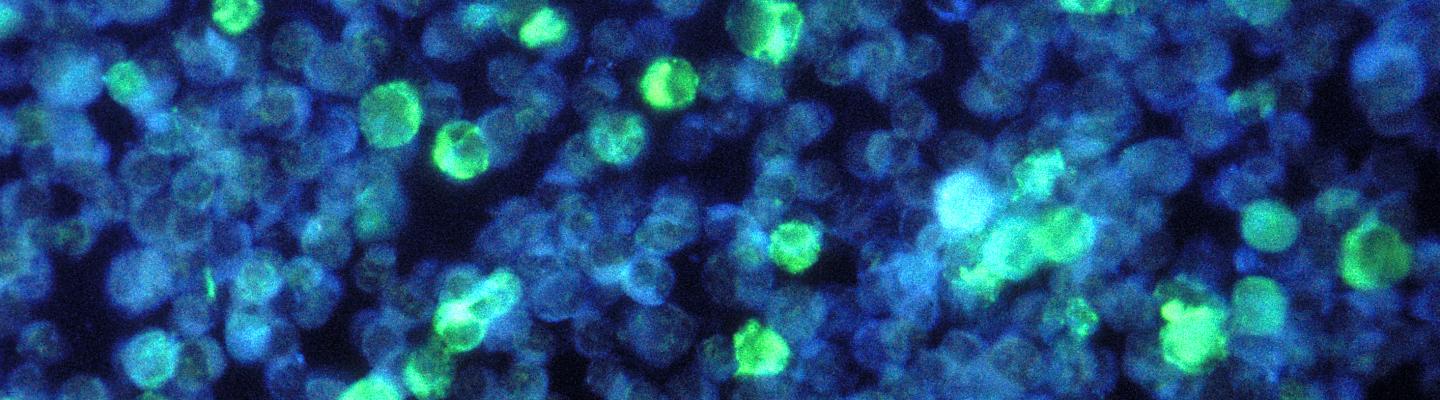
People with XLA have extremely low numbers of B cells, and blood tests will show extremely low levels of all types of immunoglobulins (antibodies). People with XLA fail to develop antibodies to specific germs and will not produce protective antibodies after immunizations. Most laboratories can examine B cell numbers in blood samples, while specialized labs can test for the BTK mutation.
Treatment
People with XLA receive intravenous (through the vein) or subcutaneous (just under the skin) immunoglobulin regularly, as well as antibiotics to treat infections. NIH researchers have improved methods to identify the specific microbes responsible for infections in people with XLA. By identifying hard-to-detect bacteria, physicians can prescribe the correct treatments.