For NIAID scientist Hans Ackerman, M.D., DPhil, and his fellow malaria researchers it was a story several years in the making and involving multiphoton molecular imaging of live human arteries; gene expression and immunoprecipitation studies; computational modelling of the interactions between two proteins—hemoglobin and the enzyme nitric oxide synthase (NOS); and functional studies of vasoregulation in isolated human arteries. What emerged from their efforts is a new and unexpected understanding of the role played by hemoglobin in regulating constriction and dilation of human blood vessels as well as insights into the links between hemoglobin gene variants, including the one that gives rise to Sickle Cell Disease, and protection from severe malaria. Their findings appear online in the journal Circulation.
Malaria as a vascular disease
Malaria parasites infect red blood cells, and it is the interaction of these infected cells with the vascular endothelium (the layer of cells lining blood vessels) that gives rise to disease symptoms and helps characterize malaria as a vascular disease, notes Dr. Ackerman. In the healthy endothelium, nitric oxide (NO, which is made by the enzyme NOS) is produced and then quenched in a carefully regulated manner, allowing blood vessels to dilate and constrict smoothly. During a malaria infection, in contrast, a series of pathological forces combine in the blood vessels, resulting in dysregulation of vasodilation, breakdown of tight junctions between cells, and leakage of fluid into the surrounding tissue. When these damaging effects occur in the brain, they may lead to cerebral malaria, coma and death.
“We don’t currently have malaria treatments that target endothelial dysregulation, but the concept of modulating nitric oxide signaling is appealing because it could potentially help restore vascular function and integrity,” says Dr. Ackerman. In studies in mice with cerebral malaria, direct administration of NO improved survival; however, the same effect was not seen in clinical trials involving children with cerebral malaria who were treated with inhalable NO. “So, we were interested in obtaining a better understanding of endothelial NO signaling with the aim of finding ways to modulate it,” Dr. Ackerman said.
Looking inside live arteries
To do this, Dr. Ackerman and his colleagues first used multiphoton microscopy to visualize hemoglobin inside live human artery samples that were obtained from healthy volunteers or from patients who were undergoing abdominal surgery. “I expected that endothelial hemoglobin would simply pervade the vessel in a kind of mist,” said Dr. Ackerman. “To our surprise, the imaging revealed that hemoglobin molecules were situated regularly throughout the stretchy elastin fibers separating the endothelial layer from the surrounding layer of smooth muscle around the artery,” he said. A 3D rendering showed hemoglobin clusters sitting in “pores” where endothelial cells connect to smooth muscle cells. These junctions are where cell-to-cell signaling, including the production of NO, happens, explains Dr. Ackerman. “It looks like hemoglobin is organized in a way to put it very close to the site of NO production, suggesting that it may play a role in regulating NO production, thus helping to reduce any off-target effects of NO,” he added.
A second surprise emerged from the multiphoton imaging: in contrast to mice, where only the alpha subunit of hemoglobin is found in the endothelium, human arteries express both the alpha and beta subunits of hemoglobin, which exists as a tetrameric—four-part—molecule. The team used immunoprecipitation to determine that alpha and beta hemoglobin subunits form a complex with endothelial NOS (along with another enzyme) that is embedded in the artery wall. When NOS produces nitric oxide, it immediately encounters the hemoglobin and is transformed into a relatively inactive chemical called nitrate that is unable to leave the endothelial cell. When hemoglobin is displaced from the endothelial NOS, however, then NO is produced and can send a signal to the smooth muscle cells that allows the vessel to dilate. Taken together, the team’s findings through these studies identified hemoglobin as a direct regulator of vasodilation and constriction in the endothelium.
Human hemoglobin variants
The investigators next sought to understand how variant forms of hemoglobin changed its ability to regulate NO production. In mice, noted Dr. Ackerman, it would be possible to selectively “knock out” the genes responsible for either alpha or beta hemoglobin subunits and observe the effects. Since this is not possible in people, the team turned to naturally occurring conditions in which either the alpha or beta hemoglobin subunit gene is mutated. First, they used live artery imaging to view blood vessel samples taken from people who have a partial deletion of the alpha globin gene, which limits the amount of alpha hemoglobin they can produce. Compared to arteries from healthy volunteers, the arteries containing the alpha globin deletion dilated more when subjected to identical constriction-causing stimuli. The interpretation is that lower levels of the alpha subunit mean the hemoglobin complex does not function to fully inhibit NO production and the NO that is produced has a greater vasodilating effect relative to that seen in healthy arteries.
The investigators then employed a 15-amino-acid-long peptide replicating the part of the alpha hemoglobin subunit that interacts with NOS. When introduced into the vessel wall, the manufactured peptide binds to the NOS enzyme, preventing the full hemoglobin-NOS complex from forming and catalyzing the chemical reaction that transforms NO to nitrate. Without the reaction, the NO produced by NOS can leave the cell and stimulate dilation.
Beta globin gets in the picture
The information about the role played by alpha subunit hemoglobin had previously been sketched out in mice, explained Dr. Ackerman, and their studies extended that understanding to humans. The next phase of the research used computational modelling to develop a picture of how alpha-beta hemoglobin forms the complex with NOS. The model shows portions of the alpha and beta amino acid chains where they come into contact with key portions of NOS enzyme. One of the most important sites of contact, the investigators saw, was where a positively charged amino acid of NOS meets the negatively charged amino acid glutamic acid in position 6 of the beta globin chain forming a stabilizing ‘salt bridge’ between the two molecules.
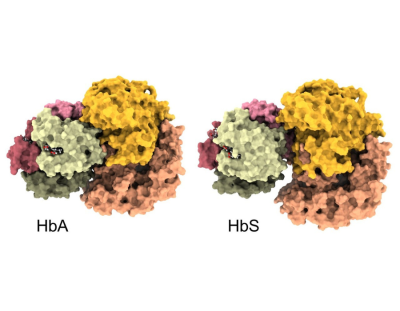
“We next generated a molecular simulation model of the complex, which shows how tightly the hemoglobin nestles into a half-moon shape of NOS,” said Dr. Ackerman. “However, if we simulate the shape of the complex after removing that single, negatively charged glutamic acid from position 6 of the beta chain, we see a gap open up between hemoglobin and NOS.”
Removing glutamic acid from position 6 of hemoglobin’s beta chain exactly replicates the situation that arises in people with Sickle Cell Disease. People who inherit two copies of the mutated gene coding for beta hemoglobin produce a form of hemoglobin, called sickle or hemoglobin S, where a different amino acid is substituted for glutamic acid in position 6, leading hemoglobin S molecules to aggregate, which distorts red blood cells into a sickle shape. People who have sickle cell trait (those have inherited a single mutated gene), which is most common in Africans and people with African ancestry, produce both normal and hemoglobin S (and do not have symptoms of Sickle Cell Disease). People with sickle cell trait are known to have some protection from severe malaria. It’s possible, says Dr. Ackerman, to explain this advantage by reference to the picture they’ve developed of the interaction between hemoglobin S and NOS: in theory, a somewhat loose connection between hemoglobin S and NOS would allow production of NO and subsequent vessel dilation, lessening the vasodilation dysregulation that characterizes severe malaria.
Next steps: finding ways to target the hemoglobin-NOS complex
Dr. Ackerman and his colleagues also synthesized a peptide that replicates the part of the beta chain where the sickle cell trait amino acid substitution occurs that alters the way hemoglobin interacts with NOS and studied its effects in isolated human arteries. They found that the mimetic peptide disrupted the hemoglobin-NOS complex, which permits NO to be produced and leave the cell, resulting in vasodilation. Unlike NO-producing nitroglycerin pills, which dilate blood vessels in a non-specific way, the synthetic beta globin peptide made by the investigators targets just the cell junctions where NO is produced, explains Dr. Ackerman. It’s possible, he adds, that such a mimetic peptide could be further developed into a treatment that could restore normal vasodilation and could be envisioned as an intervention for cases of severe malaria and other diseases where NO signaling is insufficient.
Reflecting on the odyssey of research that culminated in their new paper, Dr. Ackerman said, “These discoveries were elevated by the participation of Black individuals who were interested in learning about alpha thalassemia and sickle trait and who wanted to contribute by participating in research. Our research team included members who came from communities where thalassemia and sickle cell disease are common. This helped our team engage with study participants and develop a strong sense of purpose around our research that was essential in producing this new understanding about fundamental workings of the human body.”
Reference: SD Brooks et al. Sickle trait and alpha thalassemia increase NOS-dependent vasodilation of the human arteries through disruption of endothelial hemoglobin-eNOS interactions. Circulation DOI: 10.1161/CIRCULATIONAHA.123.066003 (2025).