Malaria, one of the deadliest infectious diseases on the planet, has had a profound impact on humanity throughout history. This disease has even left its mark in our DNA: Many scientists believe it has had a strong selective pressure on the human genome over time. Because malaria is often fatal in children, babies born with some degree of resistance to the parasite that causes malaria have a better likelihood of growing up and passing those traits along to their own children. Unfortunately, some of these traits may come at a price: For more than 50 years, scientists have documented that malaria infection is associated with high levels of autoantibodies—antibodies that recognize and attack the person’s own tissues and are associated with autoimmune disorders.
To investigate the link between autoantibodies and malaria immunity, NIAID researchers, along with their colleagues, have studied the molecular mechanisms of these malaria defense systems. Their findings, recently published in Immunity, reveal the associations between malaria, human resistance to it, and autoantibodies that are linked to certain autoimmune disorders—specifically, systemic lupus erythematosus (SLE).
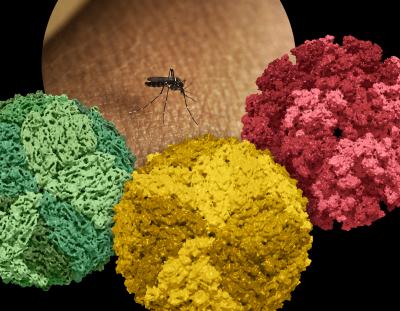
The researchers began by examining a collection of blood samples collected during a longitudinal study of 602 people, aged three months to 25 years, in the West African country of Mali. Malaria transmission is highly seasonal in Mali: the parasite which causes malaria, Plasmodium falciparum, is transmitted by mosquitoes, which need certain conditions to reproduce. During the dry season, which ends in May, malaria transmission rates are low. The researchers tested for autoantibodies in blood samples that were collected in May and then linked this with whether the participant had symptomatic malaria that needed treatment during the ensuing malaria season.
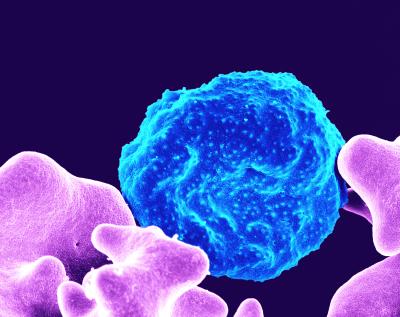
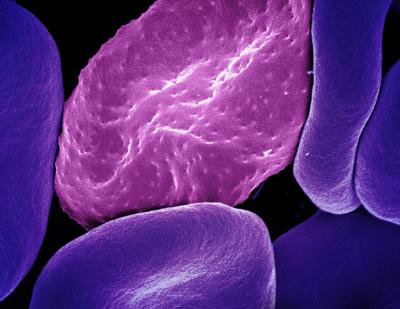
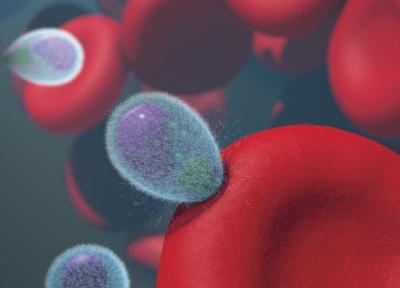
Participants who had very high levels of autoantibodies had a 41 percent lower risk of getting sick with malaria than people who had low levels of autoantibodies. To investigate how autoantibodies might protect from malaria, the researchers took blood samples with high levels of autoantibodies and isolated the autoantibodies. They then exposed malaria parasites to the autoantibodies in the laboratory and found that parasite growth was inhibited. The autoantibodies bound to proteins that the parasite uses to invade human red blood cells. The researchers believe that something similar may have happened to the participants of this study—their autoantibodies reduced the parasite’s ability to invade and grow in their blood cells, increasing their chances of remaining free of malaria symptoms.
Although this adaptation seems beneficial, it may come with a catch. Very similar autoantibodies can be found in the blood of people with SLE. This chronic autoimmune disorder can affect almost any organ system, but it often manifests as a rash, joint pain, and persistent fatigue. In its worst forms, it can be debilitating. While the causes of SLE are still unknown, it does appear to have a genetic component—for example, in the U.S., SLE is more common in some ethnic groups than others, including people with African ancestry. However, for unclear reasons, SLE and other autoimmune disorders are less common in Africa, suggesting that other factors alter the immune system to decrease the risk of autoimmune disorders there. Participants in the Mali study with high levels of autoantibodies had no symptoms of SLE or other autoimmune disorders.
When the researchers tested autoantibodies from people in the United States with SLE, they reacted to malaria parasites similar to the autoantibodies from the Malian study participants. These findings suggest that the overactive immune response that contributes to SLE may have evolved to defend against malaria. Even though many people with SLE today will never encounter a malaria-carrying mosquito, they still produce the antibodies that may have helped their ancestors survive malaria.
Reference:
Hagadorn, K et al. Autoantibodies inhibit Plasmodium falciparum growth and are associated with protection from clinical malaria. Immunity. DOI: https://doi.org/10.1016/j.immuni.2024.05.024 (2024)