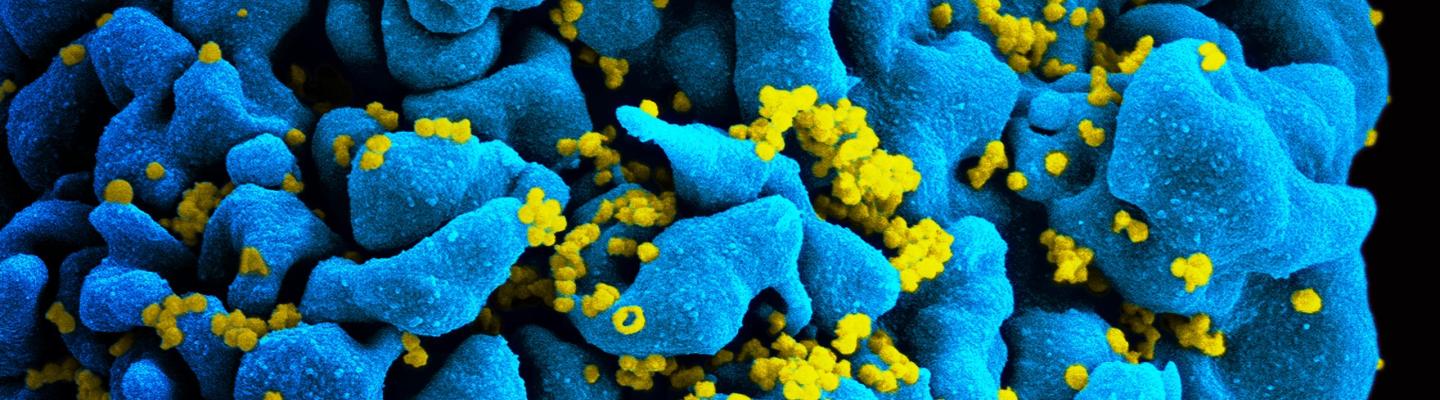
Many people living with HIV naturally develop broadly neutralizing antibodies (bNAbs), which can stop a wide range of HIV strains from infecting human cells in the laboratory but arise too late after infection to effectively fight the virus. While an experimental HIV vaccine aims to prevent infection by stimulating the immune system of an uninfected person to produce protective antibodies, passive antibody transfer involves giving bNAbs directly to an uninfected person through injections or intravenous infusions. Scientists have shown that this technique safely protects monkeys from infection with a monkey version of HIV, and studies are underway to determine whether it can protect humans from infection with HIV.
NIAID currently supports eight clinical trials of passive antibody transfer for HIV prevention involving six different bNAbs. The most advanced of these trials are called the AMP Studies, short for “antibody-mediated prevention.” Launched in 2016, the AMP Studies are two trials testing whether giving people a bNAb called VRC01 as an intravenous infusion every eight weeks is safe, tolerable, and effective at preventing HIV infection. Learn more about the AMP Studies.
Most of the bNAbs in NIAID-supported clinical trials of passive antibody transfer have been modified to lengthen the amount of time they last in the body and thereby reduce the frequency of infusions. Scientists are also selecting and developing bNAbs with greater potency and breadth to reduce the necessary dosage and dosing frequency for passive antibody transfer and to minimize the number of bNAbs that may need to be combined to protect against HIV infection. Additional research is focused on devising ways to concentrate bNAbs at the mucosal surfaces of the rectum and vagina, a critical strategy for blocking sexual transmission of HIV.
Since 2015, NIAID and the global pharmaceutical company GSK have collaborated to evaluate and improve known and novel bNAbs and to identify combinations of bNAbs capable of blocking the widest range of HIV strains. The partners are examining these bNAbs to determine which ones are the most promising for the development of long-acting tools for both HIV prevention and treatment. To learn more about the development of bNAbs for long-acting HIV treatment, read this overview of future directions for HIV treatment research.