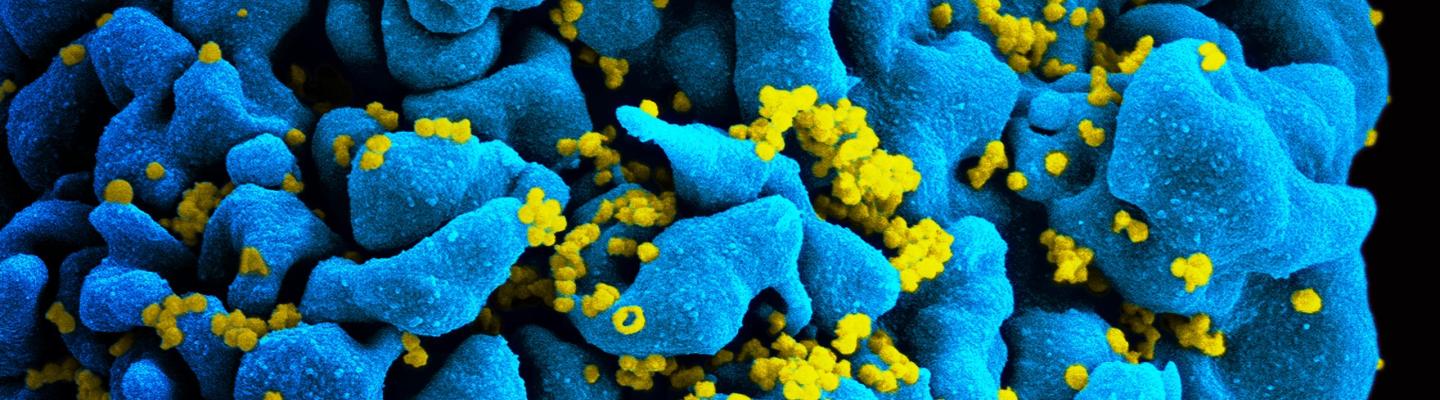
Viral eradication for HIV would involve the complete elimination of HIV from the body, including the destruction of cells infected with latent HIV. One strategy under study would deplete the HIV reservoir by prodding the virus out of its latent state so that an enhanced immune system or administered therapies can target and eliminate HIV-infected cells. An alternate strategy would be to use gene therapy to specifically excise or inactivate the latent HIV.
Reversing HIV Latency and Destroying the HIV Reservoir
Scientists are looking into strategies that induce latently infected cells to express HIV proteins on their outer surface so that an enhanced immune system or therapeutic agents can recognize these proteins and kill the infected cell. This strategy is sometimes called “kick and kill” or “shock and kill” —meaning latent HIV is drawn out by latency-reversing agents, allowing the latently infected cells to be targeted for destruction by the immune system or other anti-HIV therapy. Currently, several latency-reversing agents are under investigation in the laboratory and in human clinical trials.
Once the latent HIV begins to replicate after the “kick” stage, components of the immune system or therapeutic agents kill the HIV-infected cells to ensure a complete eradication of the latent HIV reservoir. In 2015, a team of researchers at NIAID developed a double-headed protein called VRC07-αCD3, which is a kind of bispecific T-cell engager, or BITE. One arm of this protein binds to a receptor on HIV-infected CD4 T-cells, prompting that cell to display HIV proteins on its outer membrane. In a separate step, the other arm of VRC07-αCD3 then binds to these HIV membrane proteins while the original arm attaches to a killer T-cell in order to activate it and bring it in proximity to the infected cell. The activated killer T cell then kills the infected cell.
Employing Stem Cell Transplantation and Gene Therapy
In the absence of ART, the vast majority of people living with HIV will eventually develop complications, including AIDS. However, some people living with HIV maintain low levels of virus in the blood—or viral load—even without therapy, indicating that their immune cells are protected from HIV. Other individuals claim to have had significant exposure to HIV but did not acquire the virus.
Beginning in the late 1990s, studies revealed that people with stronger natural protection from HIV tended to have mutations in the gene that codes for a protein called CCR5. CCR5 exists on the surface of human immune cells, and it is one of the proteins that HIV uses to enter and infect cells. When CCR5 is dysfunctional or absent, HIV can no longer infect immune cells. If researchers induce CCR5 dysfunction or absence by mutating the CCR5 gene in the cells of adults who do not naturally have this rare mutation, scientists may be able to help these people better control or eliminate HIV infection. Based on these findings, NIAID funds experimental genetic engineering approaches to an HIV cure.
Some clinicians have attempted to cure HIV in people who needed a bone marrow transplant to treat a life-threatening cancer by selecting a donor whose stem cells had the CCR5 mutation. If the procedure is successful and the patient survives, it can lead to a reconstitution of the immune system with cells that are impervious to HIV. This approach has succeeded only twice in curing people of HIV, although it has been tried many other times.
One of these two successful cases was known as “the Berlin patient” for many years before revealing his identity, Timothy Brown. This American man living with HIV was diagnosed with myeloid leukemia while living in Germany. Brown’s doctors determined he needed a complete bone marrow transplant, the standard treatment for his life-threatening cancer, and selected a donor who had the CCR5 mutation. Brown nearly died from the treatment. However, in the end, not only did the procedure cure his leukemia, but also it eliminated HIV from his body. In 2009, Brown’s physicians reported these findings in the New England Journal of Medicine as a case study funded by the German Research Foundation.
In 2019, researchers reported a similar case in the journal Nature. The anonymous “London patient” received a bone marrow transplant for Hodgkin’s lymphoma using stem cells from a donor with the CCR5 mutation. The patient survived the transplant, and multiple subsequent analyses revealed no evidence of HIV infection. At the time of publication, the patient’s HIV had remained in remission without ART for more than 18 months. Researchers will continue to monitor the “London patient” for the reemergence of HIV, as well as long-term health effects of the transplant. The case study was supported by the United Kingdom’s National Institute for Health Research, the Oxford and Cambridge Biomedical Research Centres and amfAR (The Foundation for AIDS Research).
While these extraordinary cases are “proof of concept” that HIV can be cured, a bone marrow transplant is a highly risky, intensive and expensive procedure performed only to treat life-threatening conditions in the absence of other treatment options. It is not a realistic way to cure HIV in the millions of people around the world who are living with the virus. Moreover, attempts to cure HIV with bone marrow transplants in other individuals have not been successful, primarily because the procedure has only been performed in patients with both HIV and blood cancers, which have a high mortality rate even after bone marrow transplants.
Other recent advancements have opened up the possibility of enhancing the immune system’s ability to fight HIV through gene-editing technologies. Clinicians employing such techniques would remove immune cells from an HIV-positive patient, use gene-editing to directly alter the CCR5 gene, and then transfuse the cells back into the individual. In this case, a donor with an advantageous CCR5 mutation is not required, and the patient does not risk life-threatening rejection of donor tissue. Some preliminary research has been done to assess gene-editing as a strategy for both HIV treatment and cure.
Some clinicians have also proposed using gene-editing technology to directly cut viral genes out of the DNA of latently infected cells. This technique would target what is called the HIV provirus. When HIV infects a cell, the virus inserts its own genome into the cell’s DNA. Advances in biotechnology make it possible for scientists to potentially locate and remove these genes from latent cells using programmed DNA-slicing enzymes. Pre-clinical studies in animals have shown that such a strategy can excise proviral DNA from infected cells. However, scientists still need to understand how to efficiently deliver these gene-editing enzymes to all cells that make up the latent HIV reservoir without causing unintended consequences that may be unhealthy for the patient. Therefore, more research needs to be done to evaluate this approach in living organisms.