NIAID-developed Vaccines May Provide Flexibility and Choice Among Ebola Vaccines
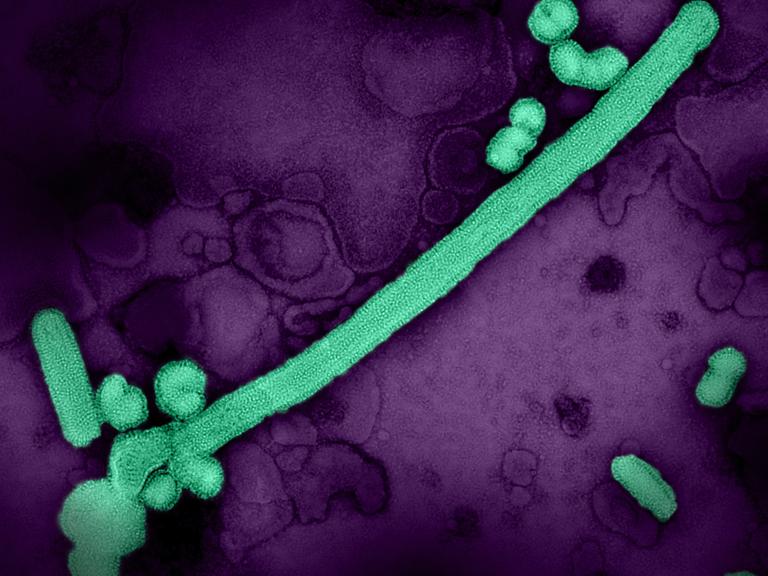
Ebola viruses cause devastating disease in people, resulting in severe and often fatal hemorrhagic fever called Ebola virus disease. Of the four species of Ebola viruses that cause disease in people, Zaire ebolavirus (EBOV) and Sudan ebolavirus (SUDV) have caused more than 30 known outbreaks in the last century, killing more than half of those with the disease. Scientists at NIAID’s Vaccine Research Center (VRC) developed novel vaccines to combat these viruses, which were advanced to clinical trials in response to the 2014-2016 Ebola epidemic in the West African countries of Guinea, Liberia, and Sierra Leone. In two phase 1/1b trials conducted in the United States and Uganda, the researchers evaluated combinations of the experimental vaccines against Ebola disease in healthy adults, finding them safe, tolerable, and capable of producing immune responses. Comparisons between the different vaccine regimens revealed important data on how the vaccines could be administered in routine and outbreak settings. The results of the trials were published last week in npj Vaccines.
In a Springer Nature Research Communities blog post published after the research article, the authors discussed how the vaccines were rapidly brought to clinical trials amid reports that cases of Ebola virus disease were spreading in Guinea in March 2014. At the time, there were no approved vaccines or therapeutics for Ebola virus disease. When outbreaks occur, Ebola virus spreads quickly, and severe symptoms and death can occur within weeks of infection. The rapid progression of Ebola virus disease in individuals often causes outbreaks to be short but deadly, although the threat of larger epidemics looms large. In 2014, the Ebola outbreak spread to Liberia and Sierra Leone, with a small number of travel-related cases in the U.S. and several African and European countries. Public health officials around the world feared the outbreak could become a global pandemic.
At the same time, researchers at the VRC were preparing to bring new investigational Ebola vaccines, called cAd3-EBO, cAd3-EBOZ, and MVA-EbolaZ, to clinical trials. The scientists and their collaborators worked hard to accelerate the process and launch a clinical trial in the U.S. to test whether a two-dose vaccine regimen could be used in the event of a prolonged outbreak. The researchers also launched a similar clinical trial in Uganda. The two trials enrolled 230 healthy people, 174 of whom had already received an Ebola vaccine in previous studies.
The trials evaluated “prime-boost” vaccine regimens, which first use a “prime” vaccine followed by a different “boost” vaccine. Each of the vaccines uses a portion of a protein from the surface of Ebola viruses called Ebola glycoprotein (GP) as the immunogen—the part of the vaccine that trains the body to generate an immune response without causing disease. The prime vaccines used in the trial were cAd3-EBOZ and cAd3-EBO, which use a vaccine vector based on a chimpanzee adenovirus not capable of replicating inside the human body, called cAd3. The cAd3 vaccines included either EBOV GP (the cAd3-EBOZ vaccine) or a combination of EBOV and SUDV GPs (the cAd3-EBO vaccine). The boost vaccine was MVA-EbolaZ, which uses EBOV GP with a different vector, modified vaccinia virus Ankara (MVA). Preclinical studies had shown the combination of vaccines could produce strong, protective immunity against Ebola virus disease in animals.
Combining the results of the U.S. and Uganda trials, the researchers found the vaccines to be safe and tolerable in people with and without prior Ebola vaccinations. Additionally, the cAd3 Ebola vaccines produced immune responses in people, stimulating the production of antibodies against Ebola that reach high levels as soon as two weeks after vaccination and lasting up to 48 weeks after the prime and boost vaccinations. The researchers also found that different time intervals between the prime and boost vaccinations influenced the magnitude of antibody and cellular immune responses.
The 2014 Ebola outbreak was larger than any previously reported. When it was declared over in 2016, the disease had claimed 11,325 lives among the 28,652 reported cases. Several clinical trials evaluating Ebola vaccines, including cAd3 vaccines, were launched at the time, providing much-needed countermeasures against this deadly disease. Since then, new vaccines against Ebola virus disease have emerged, with one approved for use in the U.S., the European Union (EU), and several African countries, and a prime-boost regimen that was authorized for use in the EU.
Given the unpredictable nature of Ebola outbreaks, several different vaccination strategies could be useful. These include routine vaccinations in regions where Ebola virus disease is known to occur, pre-exposure vaccinations of frontline workers during outbreaks, emergency vaccinations of people in outbreak zones, as well as the availability of multiple vaccines for different individuals. According to the researchers, these findings demonstrate that the cAd3 and MVA Ebola vaccines could make useful additions to countermeasures against Ebola virus disease, allowing for choice and flexibility among the currently available vaccines. Additionally, they note that the findings will inform the development of vaccine campaigns and emergency response strategies during Ebola outbreaks.
References:
M Happe, AR Hofstetter, et al. “Heterologous cAd3-Ebola and MVA-EbolaZ vaccines are safe and immunogenic in US and Uganda phase 1/1b trials.” npj Vaccines DOI: 10.1038/s41541-024-00833-z (2024).
AR Hofstetter, M Happe, et al. “Clinical Testing of the cAd3-Ebola and MVA-EbolaZ vaccines.” Springer Nature Research Communities (2024).