As syphilis rates continue to rise in the United States, emergency departments may be a way for people with limited healthcare access to get screening and treatment. A NIAID study derived an emergency department syphilis screening strategy to help people get diagnosed before their infection reaches an advanced stage. This approach could reduce disease burden and prevent cases of congenital syphilis, in which the bacteria are passed from a birth parent to their infant. The findings were published today in Open Forum Infectious Diseases.
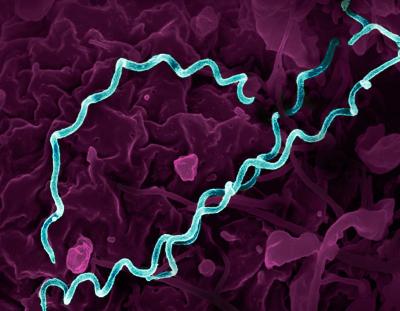
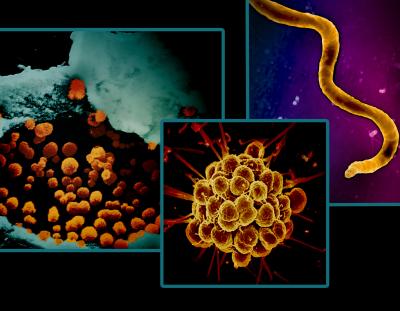
Syphilis, caused by the bacteria Treponema pallidum, is a common sexually transmitted infection (STI). Untreated syphilis can cause nervous system and organ damage, as well as pregnancy complications for birth parents and their infants. In the United States, adult and congenital syphilis cases have increased by 78.9% since 2018, with a drastic 17% increase in 2022 alone. The syphilis surge has disproportionately burdened historically and medically underserved populations. These health disparities underscore the need for greater access to syphilis testing and treatment resources.
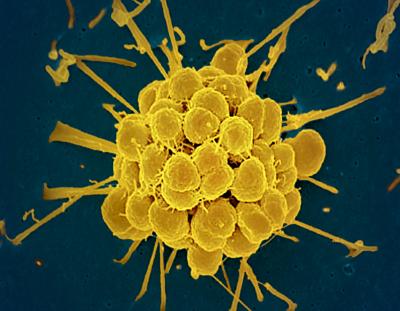
Researchers analyzed blood samples retrospectively from 1,951 adults who presented to a Baltimore emergency department over the course of a month in early 2022. They found 103 people (5.3%) had detectable treponemal antibodies to syphilis, which are indicative of a previous or active syphilis infection. Of them, 23 people (22%, 1.1% overall) had high non-treponemal antibody levels, which indicate active syphilis. The study investigators prioritized identifying people with active syphilis and performed statistical analyses to determine the associated risk factors to inform a potential screening strategy.
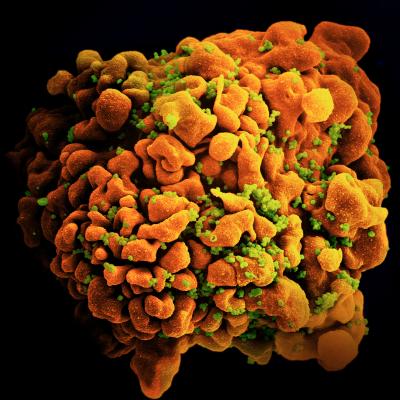
The proportion of samples with active syphilis was highest among people with HIV and people without a primary care provider. Among women with active syphilis, eight out of nine (88%) were between the ages of 18 and 49 years, which is defined as the window of reproductive age. Statistical analyses demonstrated that screening people living with HIV, without a primary care physician, and women aged 18 to 49 years would have identified 21 of the 23 people (91%) with active syphilis in the participating emergency department.
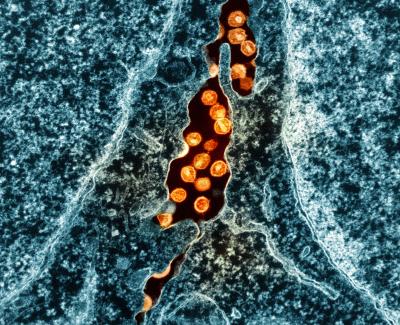
Typically, emergency departments only screen people for syphilis if they present with symptoms consistent with primary or secondary syphilis. According to the authors, the findings demonstrate the advantages of conducting focused syphilis screening during routine emergency department visits, particularly for communities who may have limited access to health care. They suggest that implementing a screening strategy informed by this study could help address the underdiagnosis of syphilis while expanding the reach of effective prevention and treatment, reducing the burden of adult and congenital syphilis. Finally, the continued syndemic of HIV and syphilis—two epidemics that interact with each other, with adverse effects on the health of communities—highlights the opportunity to provide comprehensive HIV and STI prevention and care in the emergency department, where people with high incidence frequently seek care.
Reference:
J Hunt, et al. A Potential Screening Strategy to Identify Probable Syphilis Infections in the Urban Emergency Department Setting. Open Forum Infectious Diseases. DOI: https://doi.org/10.1093/ofid/ofae207 (2024).